Researchers create a nonporous, biodegradable vascular graft
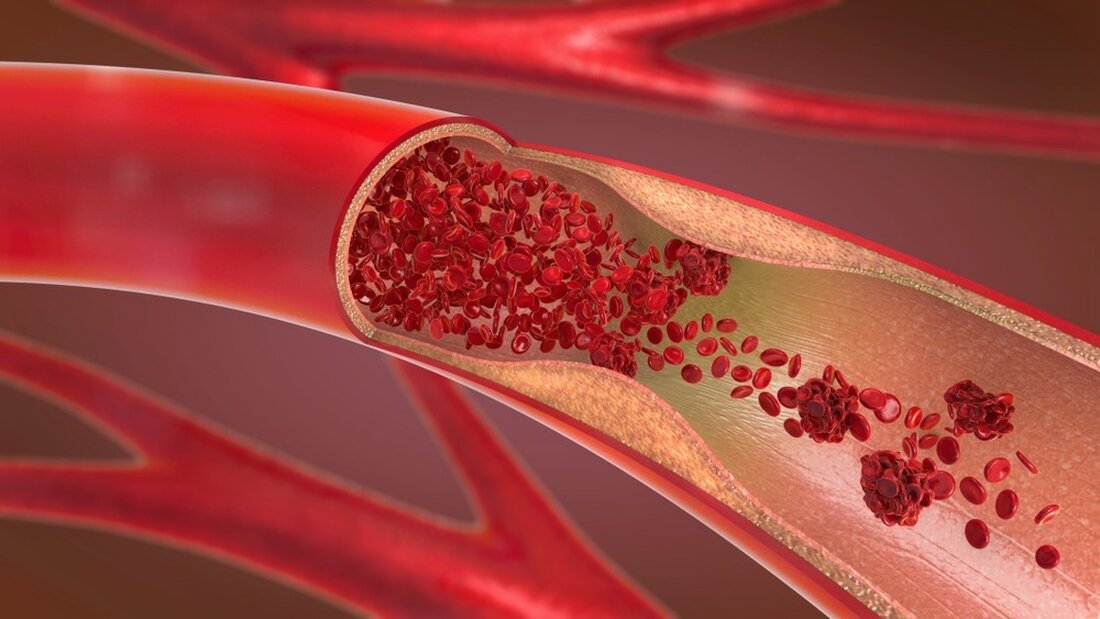
In a recently published study in Advanced Materials, a team of researchers developed a novel small-diameter biodegradable vascular graft that supports the formation of elastin-containing structures in the intima-media, which is important for the artery's normal function. Learning: Rapid regeneration of a neoartery with elastic lamellae. Image source: Christoph Burgstedt/Shutterstock Background Arterial damage caused by diseases such as severe atherosclerosis can lead to myocardial infarction and death. While autologous vascular transplants from radial arteries, internal mammary arteries or saphenous veins are ideal, patients with previous illnesses often resort to synthetic transplants. Commercially available synthetic grafts made from materials such as polytetrafluoroethylene pose problems...
Researchers create a nonporous, biodegradable vascular graft
In a recently published study in Advanced materials A team of researchers developed a novel small-diameter biodegradable vascular graft that supports the formation of elastin-containing structures in the intima-media, which is important for the normal function of the artery.

Lernen: Schnelle Regeneration einer Neoarterie mit elastischen Lamellen. Bildquelle: Christoph Burgstedt/Shutterstock
background
Arterial damage caused by diseases such as severe atherosclerosis can lead to myocardial infarction and death. While autologous vascular transplants from radial arteries, internal mammary arteries or saphenous veins are ideal, patients with previous illnesses often resort to synthetic transplants.
Commercially available synthetic grafts made from materials such as polytetrafluoroethylene pose problems such as obstruction for long periods due to blood clots and restenosis. Artery regeneration is also inhibited due to the non-biodegradable nature of these grafts.
Biodegradable vascular grafts have the advantage of increased patency and facilitation of smooth muscle cell (SMC) proliferation, endothelial formation, and deposition of extracellular matrix (ECM) proteins such as collagen and elastin. However, the long-term performance of these grafts is compromised by the improper spatial regeneration and organization of elastin fibers, leading to improper arrangement of endothelial cells and SMCs.
About studying
In the present study, researchers used a combination of tropoelastin (TE), a naturally produced ECM protein used by elastogenic cells to produce elastin, and polyglycerol sebacate (PGS), a biodegradable, highly elastic material, to create a biodegradable, nonporous vascular graft.
The TE-PGS scaffold was constructed by electrospinning to mimic the natural artery fiber structure and heat stabilized at 160 °C for 16 hours. Multiphoton microscopy was used to examine the heat-stabilized scaffold and examine the TE and PGS microstructures. The chemical conformation of the scaffold before and after heat stabilization was compared using Fourier transform infrared spectroscopy-attenuated total reflectance (FTIR-ATR).
Tensile tests were carried out to determine mechanical properties such as tensile strength, elastic modulus, elongation at break and the stress-strain curve. Mechanical stability and viscoelasticity were evaluated by subjecting the scaffold to a creep test at a load of 0.1 MPa for 500 minutes. In addition, the structural integrity and stability of the scaffold dimensions were tested by immersing the scaffold in phosphate-buffered saline at 37 °C. Long-term stability was determined based on mass change observations over 154 days after immersion.
The scaffolds were cultured with human dermal fibroblasts to determine in vitro cytocompatibility, while in vivo compatibility was measured by subcutaneously implanting the scaffold into mice and performing histological examinations at two and four weeks.
Human coronary artery smooth muscle cells (HCASMCs) and human umbilical vein endothelial cells (HUVECs) were cultured on the scaffold. The functional markers and proliferation were examined to determine whether these scaffolds would function successfully as vascular grafts.
The TE-PGS scaffolds were used to fabricate vascular grafts with diameters of 0.7, 1, and 1.5 mm and different wall thicknesses, and the burst pressure, buckling angle, and suture retention properties of these grafts were tested. The thrombogenicity of the grafts was tested before they were implanted into the infrarenal abdominal aorta of mice for eight months.
Graft degradation was monitored using immunofluorescence staining for macrophages. The distribution of elastin, collagen, SMCs, and endothelial cells was also examined, and the regenerated elastic lamellae in the intima-media were compared with those of a native mouse.
Results
The results showed that the TE50 scaffold (50:50 ratio of TE:PGS) was mechanically stable and biocompatible for use as vascular grafts and was not highly susceptible to thrombosis. It supported the proliferation of HUVEC and HCASMC and the expression of functional protein markers.
Furthermore, the nonporous nature of the TE50 scaffold stimulated the formation of structurally appropriate elastin and collagen fibers in the intima-media and adventitia, respectively. The implantation experiments in mice showed that after eight months the scaffold was completely degraded, a neoartery had formed and mature collagen was detected in the adventitia.
The elastic lamellae were surrounded by spindle-shaped, circumferentially aligned alpha-smooth muscle actin+ and smoothelin+ SMCs within eight weeks, compared to the eight months required for similar elastic lamellae to form in native mice.
Conclusions
In summary, the study described the use of a TE-PGS scaffold to construct vascular grafts that were nonporous and biodegradable and could support the proliferation of SMCs and facilitate the formation of elastin and collagen fibers.
Overall, the results showed that the TE-PGS scaffolds facilitated the formation of organized elastin lamellae, which is essential for proper arterial regeneration. Implantation testing reported biocompatibility and provided evidence of neoartery formation in mice within eight months. Additionally, the material's biodegradable nature, thermostability, tensile strength and patency make it an ideal candidate for synthetic vascular grafts.
Reference:
- Wang, Z., Mithieux, SM, Vindin, H., Wang, Y., Zhang, M., Liu, L., Zbinden, J., Blum, KM, Yi, T., Matsuzaki, Y., Oveissi, F., Akdemir, R., Lockley, KM, Zhang, L., Ma, K., Guan, J., Waterhouse, A., Pham, NTH, Hawkett, BS, & Shinoka, T. (2022). Schnelle Regeneration einer Neoarterie mit elastischen Lamellen. Fortgeschrittene Materialien, 2205614. doi: https://doi.org/10.1002/adma.202205614 https://onlinelibrary.wiley.com/doi/10.1002/adma.202205614
.

 Suche
Suche
 Mein Konto
Mein Konto
