Overview of the role of neutrophils in systemic autoimmune and autoinflammatory diseases
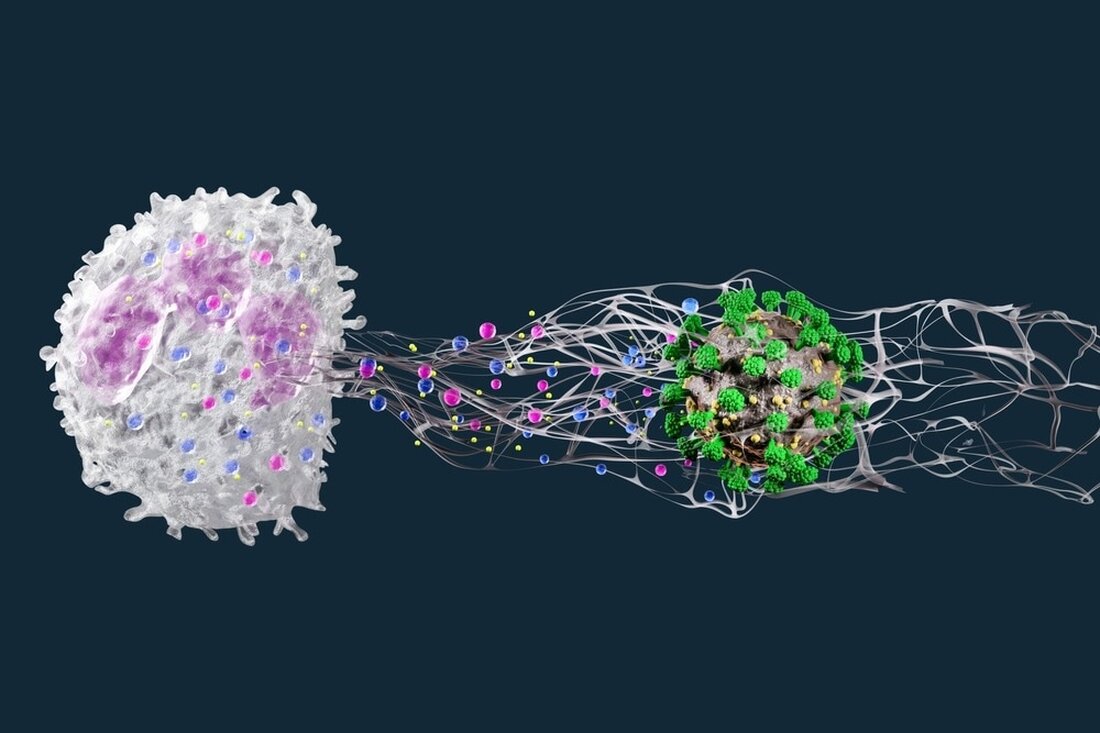
In a recent Nature Reviews Immunology journal study, researchers evaluate the role of neutrophil extracellular traps (NETs) in systemic autoimmune and autoinflammatory diseases. Learning: Extracellular neutrophil traps in systemic autoimmune and autoinflammatory diseases. Image source: Luca9257 / Shutterstock.com Background Recent research has shown that neutrophils, particularly NETs released upon activation, play a critical role in the development and progression of systemic autoimmune diseases and in the development of complex inflammatory responses that cause organ damage. Through the dysregulated cell death of neutrophil cells, autoantigens can be modified and presented to the adaptive immune system. Thanks to novel technologies that enable better assessment of neutrophils, the complexity...
Overview of the role of neutrophils in systemic autoimmune and autoinflammatory diseases
In a current one Nature Reviews Immunology In a journal study, researchers evaluate the role of extracellular neutrophil traps (NETs) in systemic autoimmune and autoinflammatory diseases.
Learn: Extracellular neutrophil traps in systemic autoimmune and autoinflammatory diseases.Image source: Luca9257 / Shutterstock.com
background
Recent research has shown that neutrophils, particularly NETs, released upon activation, play a critical role in the development and progression of systemic autoimmune diseases and in the development of complex inflammatory responses that cause organ damage.
Through the dysregulated cell death of neutrophil cells, autoantigens can be modified and presented to the adaptive immune system. Thanks to novel technologies that enable better assessment of neutrophils, the complexity of neutrophil biology and its dysregulation can now be better understood.
NETs in systemic autoimmune diseases
In systemic autoimmune diseases, the immune system cannot distinguish between itself and non-self and responds to and damages multiple tissues and organs, including joints, kidneys and blood vessels.
Numerous studies have linked neutrophils to the pathogenesis of systemic autoimmunity. In both human and animal disease models, these immune cells are often located at areas of tissue inflammation, where they support the inflammatory response.
In particular, the formation of NETs has attracted attention due to its association with autoimmunity. Many of the autoantigens produced by neutrophils in NETs, including double-stranded deoxyribonucleic acid (DNA), citrullinated peptides, histones, myeloperoxidase (MPO), and proteinase 3 (PRTN3), are known to be targeted by the adaptive immune system, as seen in systemic autoimmunity.
Systemic lupus erythematosus (SLE)
SLE is a systemic autoimmune disease with a strong type I interferon response that exhibits high autoreactivity toward nucleic acids and other nuclear and intracellular components. Skin, synovial joints, kidneys, lungs, blood vessels and heart are some of the many organs affected by this widespread inflammation, making it a classic systemic autoimmune disease.
As the condition worsens, neutrophil-specific gene expression is increased in the neutrophil populations of SLE patients compared to healthy controls. In addition, neutrophils from people with SLE exhibit abnormal oxidative metabolism, increased apoptosis, and reduced phagocytic clearance.
Compared to NETs produced from normal density neutrophils, low-density granulocytes (LDGs) from individuals with SLE show a higher propensity to produce NETs ex vivo. They have higher concentrations of modified autoantigens and immune-stimulating molecules.
Rheumatoid arthritis
As the most common systemic autoimmune disease, rheumatoid arthritis represents a major burden for patients and society. This disease not only often affects extra-articular tissues such as the lungs and the vascular system, but also particularly affects the synovial joints, which can lead to significant disabilities if inadequately treated.
Because neutrophils produce enzymes such as peptidylarginine deiminase 4 (PAD4), which catalyze the conversion of arginine to citrulline, they are a major source of citrullinated antigens. Especially in the early stages of the disease, patients with rheumatoid arthritis have an abundance of neutrophils in their inflamed joints, which can locally produce NETs.
Patients with rheumatoid arthritis have increased levels of NETs in the blood, which correlate with levels of anti-citrulline protein antibodies (ACPAs) and other systemic inflammatory markers.
Neutrophils in systemic autoinflammation
Inflammatory responses primarily affect innate immune cells such as neutrophils, which are the main cause of autoinflammatory diseases. Recent studies suggest that accurately distinguishing between autoinflammation and autoimmunity can be challenging. Rather than two separate events, these processes may be the extremes of an inflammatory spectrum.
Adenosine deaminase 2 deficiency
Adenosine deaminase 2 (ADA2) is a protein responsible for the degradation of extracellular adenosine and is mainly expressed by myeloid cells. Adenosine deaminase deficiency (DADA2) is characterized by monogenic vasculitis caused by a biallelic mutation in the ADA2 gene.
DADA2 has a variety of clinical manifestations, including vasculitis and autoinflammation. In addition, due to the lower protein activity of the ADA2 mutation, extracellular adenosine levels increase, which may lead to the development of NETs by binding to neutrophil A1 and A3 adenosine receptors.
People suffering from DADA2 also have higher levels of circulating LDGs, which can form NETs. Compared to NETs derived from healthy controls, these NETs cause macrophages to produce more inflammatory chemicals such as tumor necrosis factor (TNF), which may be due to variations in the molecular composition of the NETs.
PAPA syndrome
Pyogenic arthritis, pyoderma gangrenosum, and acne syndrome (PAPA) can manifest in a variety of ways, including arthritis involving sterile joint accumulation of neutrophils. This condition is commonly diagnosed in children.
Several studies have found increased NET production and decreased NET clearance in neutrophils from patients with PAPA syndrome. Furthermore, neutrophils in patients with PAPA syndrome are more responsive to interleukin 1 (IL-1) compared to neutrophil levels in healthy controls. Incubation of these neutrophils with anakinra, an IL-1 receptor antagonist, can suppress NET formation.
In skin biopsies from patients with PAPA syndrome, NET remnants have been found that have invaded the skin and are associated with inflammatory cytokines and increased neutrophil transcriptional responses. Overall, an association between IL-1 and dysregulated neutrophil responses in the pathogenesis of PAPA syndrome has been reported.
Conclusions
The current study reports that neutrophils have an important function in various inflammatory diseases. By targeting tissues to promote an inflammatory environment and producing neoepitopes, neutrophils play a critical role in the initiation and progression of autoimmune diseases.
Reference:
- Wigerblad, G., Kaplan, MJ (2022). Extrazelluläre Neutrophilenfallen bei systemischen Autoimmun- und autoinflammatorischen Erkrankungen. Nature Reviews Immunologie. doi:10.1038/s41577-022-00787-0
.

 Suche
Suche
 Mein Konto
Mein Konto

