Examination of plasma signatures of platelet-derived proteins in acute pulmonary embolism
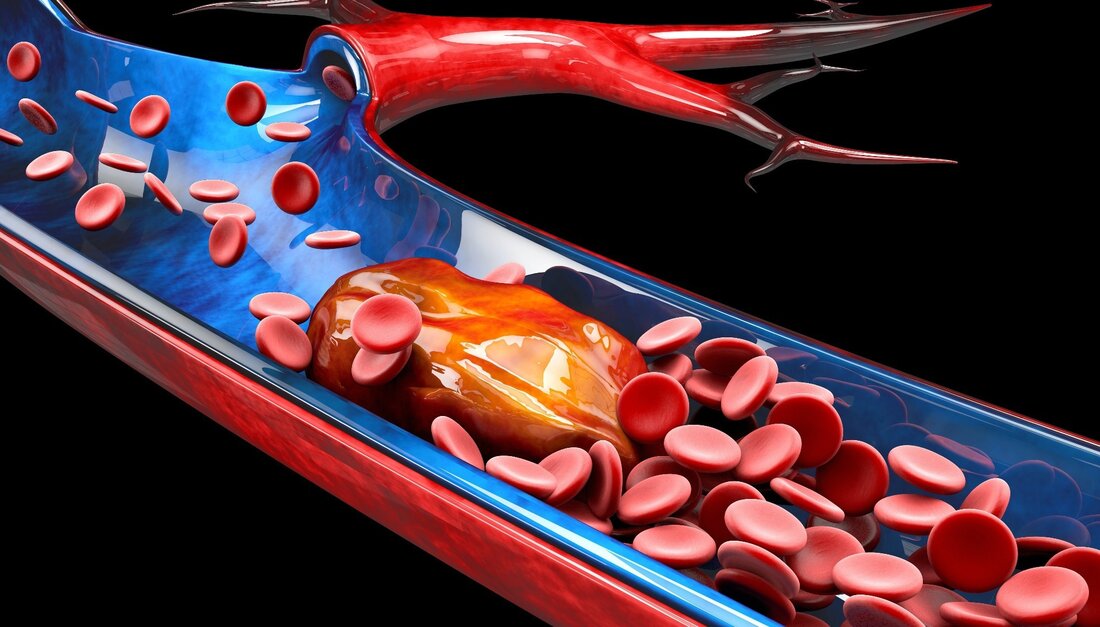
In a recent study published in Thrombosis Research, researchers determined plasma signatures of platelet-related or derived proteins in acute isolated pulmonary embolism (iPE) and deep vein thrombosis-associated PE (DVT-PE) compared to isolated DVT (iDVT). Learning: Subtype-specific plasma signatures of platelet-related protein release in acute pulmonary embolism. Image source: Victor Josan/Shutterstock Background The two primary subtypes of PE are iPE and DVT-PE, and studies have shown that plasma protein profiles differ for these two diseases. Platelets act as cellular linkers and facilitate inflammatory crosstalk between immune and endothelial cells during high arterial shear stress. This process involves…
Examination of plasma signatures of platelet-derived proteins in acute pulmonary embolism
In a recent study published in Thrombosis research, researchers determined plasma signatures of platelet-related or derived proteins in acute isolated pulmonary embolism (iPE) and deep vein thrombosis-associated PE (DVT-PE) compared to isolated DVT (iDVT).
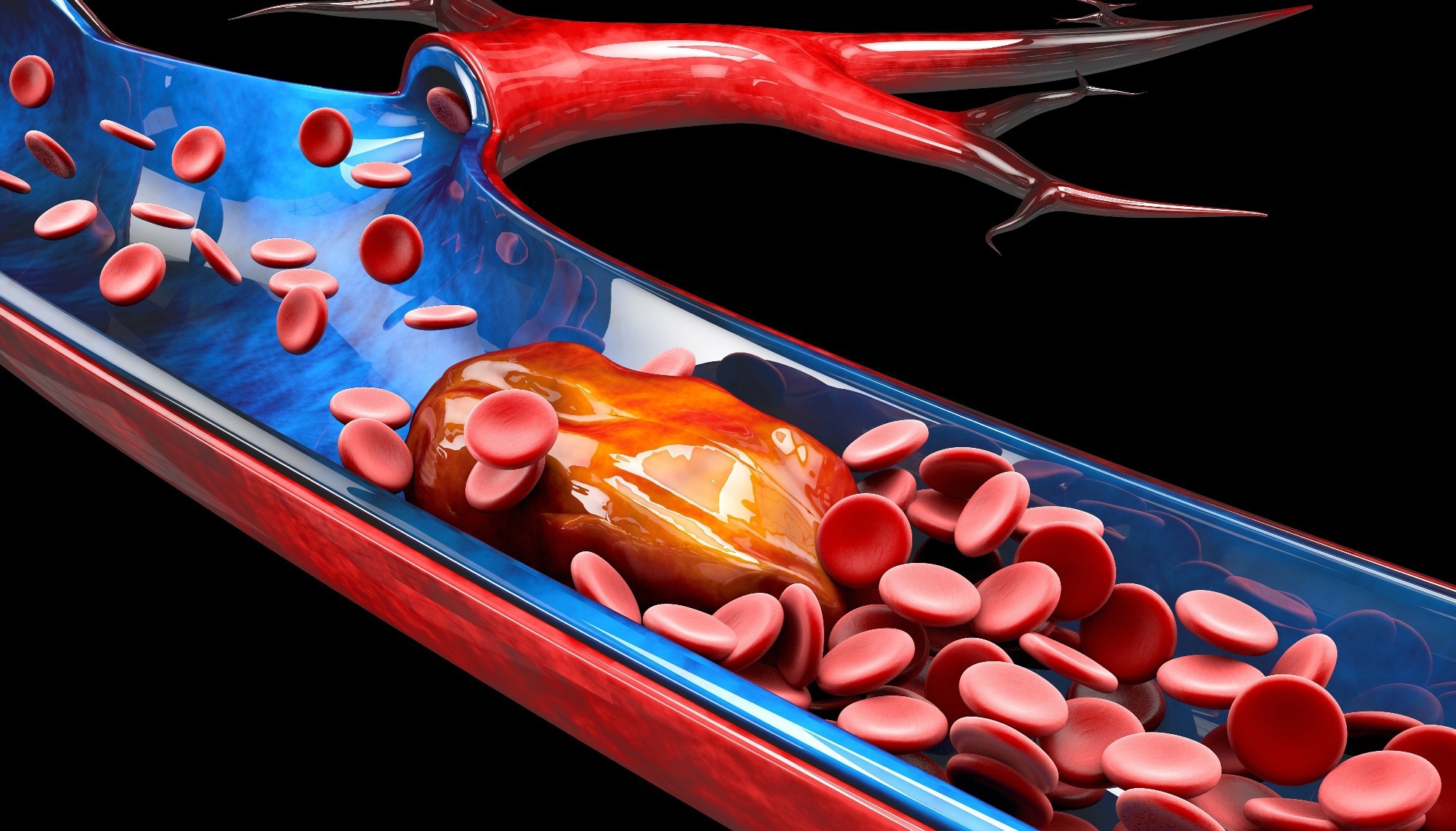
Lernen: Subtypspezifische Plasmasignaturen der thrombozytenbezogenen Proteinfreisetzung bei akuter Lungenembolie. Bildquelle: Victor Josan/Shutterstock
background
The two primary subtypes of PE are iPE and DVT-PE, and studies have shown that plasma protein profiles differ for these two diseases. Platelets act as cellular linkers and facilitate inflammatory crosstalk between immune and endothelial cells during high arterial shear stress. This process involves a direct receptor-mediated interaction between pro-inflammatory molecules and extracellular vesicles (EVs). However, local inflammatory responses at the endothelium under low shear stress activate platelets to trigger the development of venous thromboembolism (VTE) and its subtypes, including PE and DVT. The mechanisms controlling this process are less well understood.
Experimental data suggest that platelets contribute to thromboinflammation in the venous system by triggering inflammatory and coagulation processes. For example, using the VTE mouse model, researchers have shown that platelets interact with von Willebrand factor (VWF)-exposed endothelial cells and form conjugates with leukocytes via the glycoprotein (GP) Ibα, as well as triggering endothelial recruitment and leukocyte-dependent coagulation.
Human experiments have demonstrated different characteristics of platelet activation and reactivity in acute VTE. For example, platelets from patients with acute VTE showed greater exocytosis of dense granules and lysosomes. This was associated with higher plasma levels of thromboxane B2 but lower platelet-dependent thrombin formation than in patients with excluded VTE, regardless of aspirin therapy.
Mass spectrometry (MS) studies have detected over 3700 proteins in quiescent, inhibited and activated highly purified human platelets. Advanced enzyme-linked immunosorbent assay (ELISA)-based assays using MS could enable qualitative assessment of platelet-released proteins in plasma and isolated platelets. However, a more detailed analysis of platelet-associated plasma proteins in large VTE cohorts is lacking.
About the study
In the present multicenter prospective cohort study, researchers examined plasma from 541 VTE patients using machine learning-based analysis. The aim was to identify plasma protein signatures for putative platelet release specific to iPE and DVT-PE. These patients had acute VTE at the time of admission, as diagnosed by imaging. While there were 99 iPE patients, 282 were DVT-PE patients, and the team compared their data with that of 160 iDVT patients. The team used full-leg color Doppler ultrasound and computed tomography (CT) pulmonary angiography to diagnose DVT and PE. Board-certified angiologists and radiologists assessed and validated all study diagnoses.
They collected study samples as part of the Genotyping and Molecular Phenotyping of Venous Thromboembolism (GMP-VTE) project conducted in Germany. The researchers used proximity extension assay (PEA) technology for high and low plasma protein profiling from samples stored at -80°C. PEA determined normalized expression values (NPX) for all tested plasma proteins involving oligonucleotide-labeled antibodies and quantitative real-time polymerase chain reaction (PCR) amplification.
The test panel included 444 proteins identified from five databases [e.g., Kyoto Encyclopedia of Genes and Genomes (KEGG) and Gene Set Enrichment Analysis (GSEA) databases]. After comparing, the team ultimately identified 135 platelet-related proteins in the five PEA panels for further analysis.
Study results
The study cohort showed a higher prevalence of arterial hypertension, diabetes and chronic inflammatory, atherosclerotic and cardiovascular diseases in iPE and DVT-PE compared to iDVT. The higher levels of C-reactive protein (CRP), troponin I, and N-terminal (NT) prohormone B-type natriuretic peptide (NT-proBNP) similarly reflected the greater cardiovascular burden in PE subtypes.
The prescription patterns for medication were correspondingly different. For example, platelet aggregation inhibitors, i.e. acetylsalicylic acid (ASA) and clopidogrel, were overrepresented in PE patients. One explanation is that prophylactic antiplatelet agents are prescribed in patients with acute PE due to suspected myocardial infarction. It is also possible that there is a difference in platelet activity between PE and iDVT patients because the proportion of antiplatelet agents is higher in the PE groups.
Machine learning analysis of 135 extracted platelet proteins by the least absolute shrinkage and selection operator (LASSO)-regulated logistic regression models selected 24% and 22% for iPE and DVT-PE, respectively, reflecting different protein profiles compared to iDVT. Notably, all 135 platelet proteins showed good association with six platelet activation markers, supporting their likely platelet origin in the plasma of patients with acute PE compared to iDVT patients, analyzed via the PEA panels. In contrast to iPE, stromal cell-derived factor 1alpha (SDF-1α) was more highly expressed in DVT-PE than in iDVT patients, suggesting a possible special role in vascular inflammation and atherogenesis.
In iPE, compared to iDVT, protein-protein interaction (PPI) network analysis resulted in four clusters of up to six functionally interacting proteins based on 22 specifically expressed platelet-related proteins. The main cluster was associated with glue, pattern recognition and immune receptor signaling. These included the Src family kinases (SFK) c-Src, which transmit ligand signals via the immunoreceptor tyrosine-based activation motif (ITAM)-associated platelet receptors (e.g. glycoprotein VI [GPVI]).
Compared to iPE, DVT-PE presented a cluster of nine directly interacting plasma proteins associated with platelets involved in tissue remodeling and leukocyte trafficking. The tissue inhibitors of matrix metalloproteinases 1 (TIMP1) and TIMP4, important effectors of tissue remodeling, were more highly expressed in DVT-PE than in iDVT and were secreted from platelet α-granules.
The authors found that higher plasma levels of both tissue inhibitors of TIMP1 and TIMP4 were associated with type 2 diabetes, arterial hypertension and myocardial infarction, consistent with the higher prevalence of major cardiovascular events in DVT-PE compared to iDVT.
Conclusions
The current study results showed that both PE subtypes had specific plasma protein profiles associated with platelets. For example, the study distinguished higher expression of P-selectin in the plasma of DVT-PE patients compared to iDVT, suggesting an association with DVT disease severity. Interestingly, thrombin peak height and spontaneous platelet aggregation in platelet-rich plasma were negatively associated in iPE compared to the iDVT phenotype. These results suggest that lower platelet reactivity in vitro may be associated with higher platelet activation in vivo during the acute phase of PE compared to iDVT. More importantly, these results suggest that while PE subtypes share some commonalities, they also exhibit distinct platelet activation patterns.
This study did not address the quantification and characterization of EV in plasma of VTE phenotypes. In cancer patients, VTE may be associated with increased plasma levels of microparticles. However, a significant increase in platelet-derived microparticles was only observed in recurrent VTE in non-cancer patients compared to healthy blood donors. Future studies should clarify the distribution of EV in the different VTE phenotypes. Further studies are also needed to specify the influence of different cell types on the release of platelet-derived proteins in PE.
In summary, the study data suggested that iPE and DVT-PE had specific but different plasma signatures involved in platelet-related immune thrombosis and thromboinflammatory processes compared to iDVT. Furthermore, platelet activation protein profiles appeared to differ between PE subtypes, with a predominance of secreted proteins in DVT-PE compared to proteins that are more likely to be released into plasma by EV in iPE. Overall, platelets contribute to the regulation of different plasma protein levels in the acute phase of PE, which vary depending on the PE subtype.
Reference:
- Gaukhar Baidildinova, Vincent ten Cate, Markus Nagler, et al. (2022). Subtypspezifische Plasmasignaturen der thrombozytenbezogenen Proteinfreisetzung bei akuter Lungenembolie. Thromboseforschung. doi: https://doi.org/10.1016/j.thromres.2022.10.005 https://www.sciencedirect.com/science/article/abs/pii/S0049384822004157
.

 Suche
Suche
 Mein Konto
Mein Konto
