Study develops a strategy for non-invasive tracking of tumor-associated macrophages
A study from Ludwig Cancer Research has developed a strategy to noninvasively track immune cells called macrophages in brain and breast tumors in living mice. Cancers often recruit and reprogram these tumor-associated macrophages (TAMs) to support their own growth and generate resistance to therapies. Led by Johanna Joyce and Davide Croci from Ludwig Lausanne and their colleague at the University Hospital of Lausanne, Ruud B. van Heeswijk, the study appears in the current issue of Science Translational Medicine and is featured on the cover of the journal. Monitoring macrophages has the potential to significantly improve the therapeutic treatment of various cancers...
Study develops a strategy for non-invasive tracking of tumor-associated macrophages
A study from Ludwig Cancer Research has developed a strategy to noninvasively track immune cells called macrophages in brain and breast tumors in living mice. Cancers often recruit and reprogram these tumor-associated macrophages (TAMs) to support their own growth and generate resistance to therapies. Led by Johanna Joyce and Davide Croci from Ludwig Lausanne and their colleague at the University Hospital of Lausanne, Ruud B. van Heeswijk, the study appears in the current issue of Science Translational Medicine and is featured on the cover of the journal.
Monitoring macrophages has the potential to significantly improve the therapeutic treatment of various cancers. Brain malignancies, which are among the deadliest primary cancers and metastases, particularly rely on the presence of macrophages, and targeting these immune cells could represent a key strategy for their treatment.”
Johanna Joyce, Ludwig Lausanne
The Joyce lab has been studying for several years the critical role that TAMs and other immune cells play in tumors that originate in the brain or metastasize there from elsewhere, such as the breast, lung or skin. For example, she and her colleagues have shown how drugs that block the action of a factor essential for macrophage growth can reprogram TAMs from a cancer-supporting state to a cancer-killing state. They discovered how the brain's resident macrophages, microglia, and those attracted to tumors from the bloodstream—monocyte-derived macrophages (MDMs)—differently populate gliomas and brain metastases. Their studies have also shown how TAMs contribute to brain tumor recurrence and resistance to therapy and identified strategies to address each of these challenges.
The ability to track changes in macrophage number and distribution over time could therefore do much to improve the management of brain tumor therapy. But that's easier said than done. Currently, the immune landscape of gliomas can only be viewed through biopsy, which-; Aside from being very invasive and therefore far from routine; allows only a glimpse of a small section of a tumor at a specific point in time.
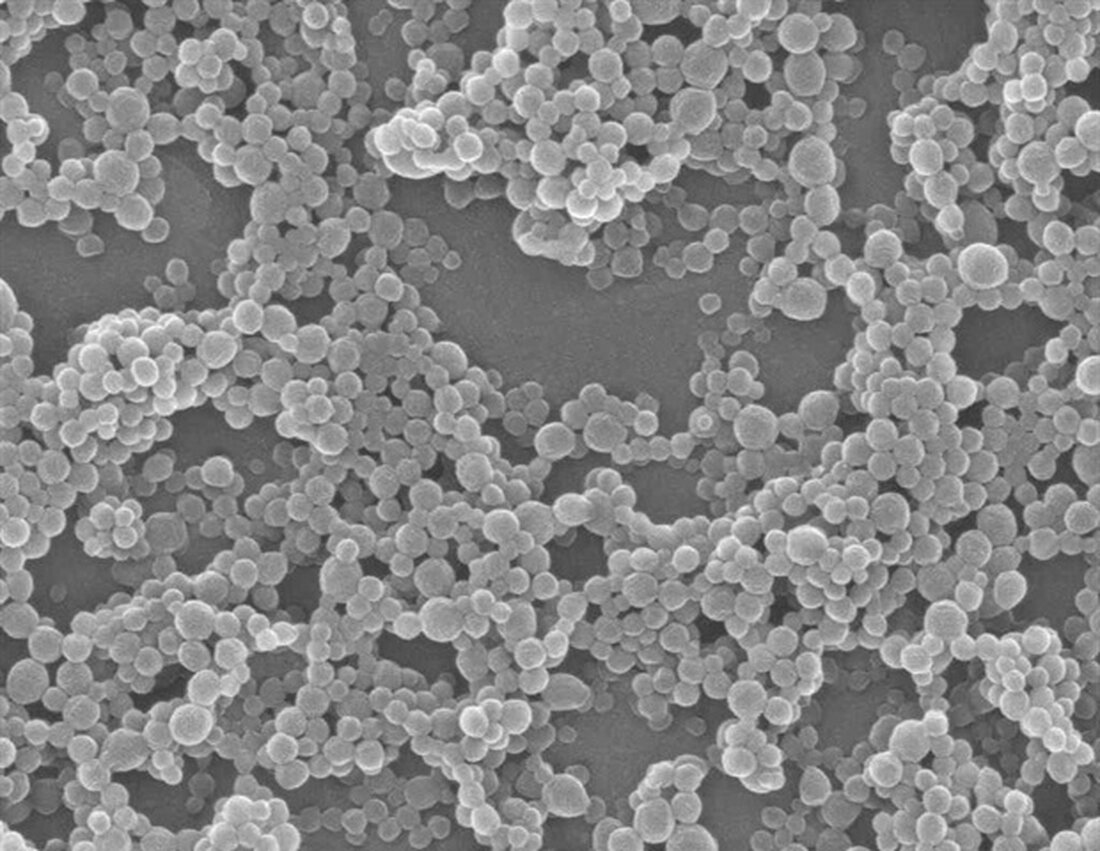
To noninvasively study TAM populations over time, Joyce and her colleagues exploited a basic function of immune cells, which is to travel throughout the body and suck up particulate matter. They injected mouse models of gliomas, breast cancer and mammary brain metastases with two different types of nanoparticles, both labeled with a fluorine isotope (19F), each emitting a characteristic and recognizable signal that could be detected by magnetic resonance imaging (MRI). ;a standard imaging technology for cancer treatment. The signals emitted by these nanoparticles are also different from those of a hydrogen isotope (1H) used to image tissue, including cancerous tumors.
The researchers show that the nanoparticles accumulate in TAMs, enabling a direct and non-invasive method to use “multispectral” MR imaging to determine not only the frequency but also the location of immune cells in the geography of tumors. For example, their imaging revealed that the labeled TAMs cluster around the leaky, malformed blood vessels created by tumors, a discovery that could have implications for combination therapies in development that aim to normalize the tumor vasculature to improve drug delivery.
Radiation therapy is a standard treatment for gliomas, and recent research from the Joyce laboratory has shown that it significantly alters the total number and types of TAMs after initial radiation and at disease recurrence. In the current study, Joyce, Croci, van Heeswijk and colleagues confirmed that although microglia and MDMs are present in approximately equal numbers in untreated gliomas, MDMs tend to take over and cluster at some distance from microglia in tumors that recur after radiation therapy.
“Imaging revealed previously unknown niches for TAMs in untreated, quiescent and recurrent gliomas,” says Joyce. "It was also recorded how the distribution of TAMs differs between gliomas and brain metastases. The imaging approaches developed in this study, if further developed, could help physicians noninvasively identify brain tumor types, better monitor prognosis and drug resistance, and thus improve therapeutic management." Brain tumors.”
Additionally, these strategies will offer scientists insight into the changing immune landscape of tumors and provide insights critical to the development of new cancer therapies.
Source:
Ludwig Institute for Cancer Research
Reference:
Croci, D., et al. (2022) Multispectral Fluorine-19 MRI enables longitudinal and noninvasive monitoring of tumor-associated macrophages. Scientific translational medicine. doi.org/10.1126/scitranslmed.abo2952.
.

 Suche
Suche
 Mein Konto
Mein Konto
