Monkeypox in the WHO European Region: epidemiological characteristics, disease severity and the impact of smallpox vaccination
The first detection and transmission of monkeypox virus (MPXV) outside its endemic areas in May 2022 was followed by a huge outbreak in several countries worldwide. As of August 23, 2022, a total of 42,807 cases have been reported along with 12 deaths in 97 Member States belonging to six World Health Organization (WHO) regions. It was declared a Public Health Emergency of International Concern (PHEIC) by the WHO Director on July 23, 2022. Learning: A large multi-country monkeypox outbreak in 41 countries in the WHO European Region, March 7 to August 23, 2022. Photo credit: Dotted Yeti/Shutterstock A new study published in Eurosurveillance aimed...

Monkeypox in the WHO European Region: epidemiological characteristics, disease severity and the impact of smallpox vaccination
The first detection and transmission of monkeypox virus (MPXV) outside its endemic areas in May 2022 was followed by a huge outbreak in several countries worldwide. As of August 23, 2022, a total of 42,807 cases have been reported along with 12 deaths in 97 Member States belonging to six World Health Organization (WHO) regions. It was declared a Public Health Emergency of International Concern (PHEIC) by the WHO Director on July 23, 2022.
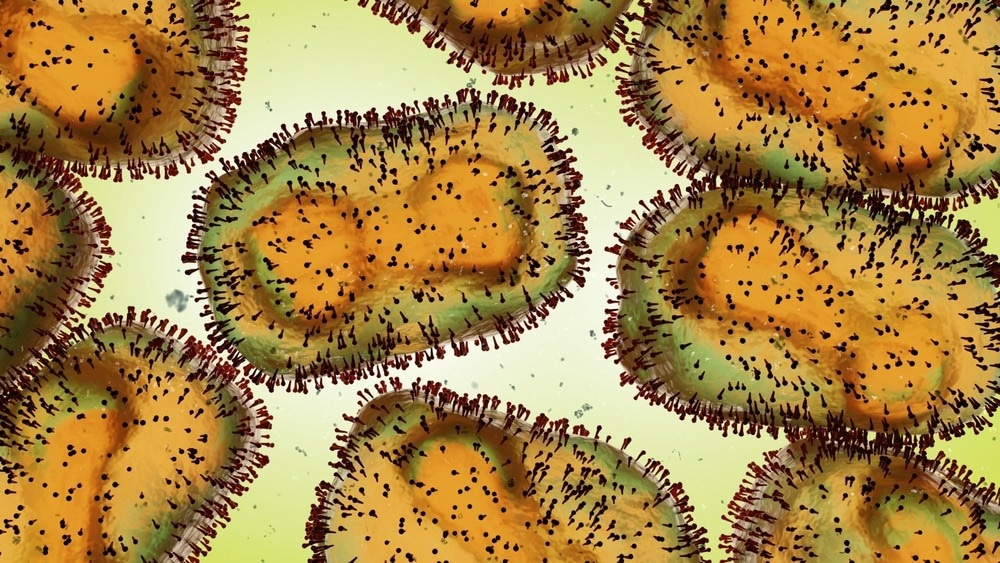
Lernen: Ein großer Ausbruch von Affenpocken in mehreren Ländern in 41 Ländern der Europäischen Region der WHO, 7. März bis 23. August 2022. Bildnachweis: Dotted Yeti/Shutterstock
A new study published in Euro surveillance aimed to analyze the epidemiological characteristics of MPX, the severity of the disease and the impact of smallpox vaccination on all cases of infection reported in the WHO European Region.
About studying
The study was carried out using data submitted to the European Surveillance System (TESSy). Nowcasting of TESSy data was performed up to 17 days before the last reported symptom to understand the current epidemiological situation.
Study results
The first non-travel-associated familial cluster of MPX cases was reported to WHO on May 13, 2022 by the United Kingdom (UK), after which it was reported in other neighboring countries. The MPXV cases were found to be caused by clade II (formerly the West African clade) and most commonly affected men who have sex with men (MSM). Europe remained the epicenter of this outbreak until the end of July.
Of the total 21,098 cases detected in the WHO European Region, 20,690 cases provided case-related data, most of which were laboratory confirmed. Nowcasting results suggested an overall plateau in cases with some differences between countries. Additionally, most cases were men with an average age of 37 years. Among them, 96.9% self-identified as MSM, while 37.2% were HIV positive. Very few cases have been reported in children and women.
The most common symptoms were skin rashes along with at least one systemic symptom such as fatigue, fever, myalgia, headache, or chills. 48.1% of cases reported the appearance of skin rashes in the anogenital region. In addition, 6% of cases were reported to require hospitalization, with three requiring admission to an intensive care unit (ICU). Of these three cases, two died of encephalitis.
Additionally, the hospitalization ratio has been reported as 10 per 1,000 cases, with younger cases having a higher risk of hospitalization. In terms of transmission routes, sexual contact was the most likely route, followed by person-to-person or fomite transmission. Exposure in pubs and in households has also been reported to play a role in transmission. Additionally, 64 of the cases were observed among healthcare workers, of which 62 were male and 55 were MSM.
Regarding smallpox vaccination, most cases reported nonvaccination before and during this outbreak, 423 reported vaccination before the outbreak, and 42 reported post-exposure preventive vaccination (PEPV). In contrast, one reported primary preventive (pre-exposure) vaccination (PPV). However, it was observed that the effects of smallpox vaccination were not entirely significant.
Therefore, the current study showed the pattern of virus transmission, the population at risk, and the impact of vaccination. However, strong interaction between health authorities, communities and international health organizations is required to manage the current outbreak of MPXV infections.
restrictions
The study has certain limitations. First, the completeness of the data submitted to TESSy may vary and depends on the availability of national data. Second, the clinical data submitted to TESSy does not reflect the full course of the disease. Finally, the nowcasting estimates could be uncertain.
Reference:
- Vaughan, A. et al. (2022) „Ein großer Ausbruch von Affenpocken in mehreren Ländern in 41 Ländern der Europäischen Region der WHO, 7. März bis 23. August 2022“, Eurosurveillance, 27(36). doi: 10.2807/1560-7917.es.2022.27.36.2200620. https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2022.27.36.2200620
.

 Suche
Suche
 Mein Konto
Mein Konto
