CAR T-cell therapy for colorectal cancer
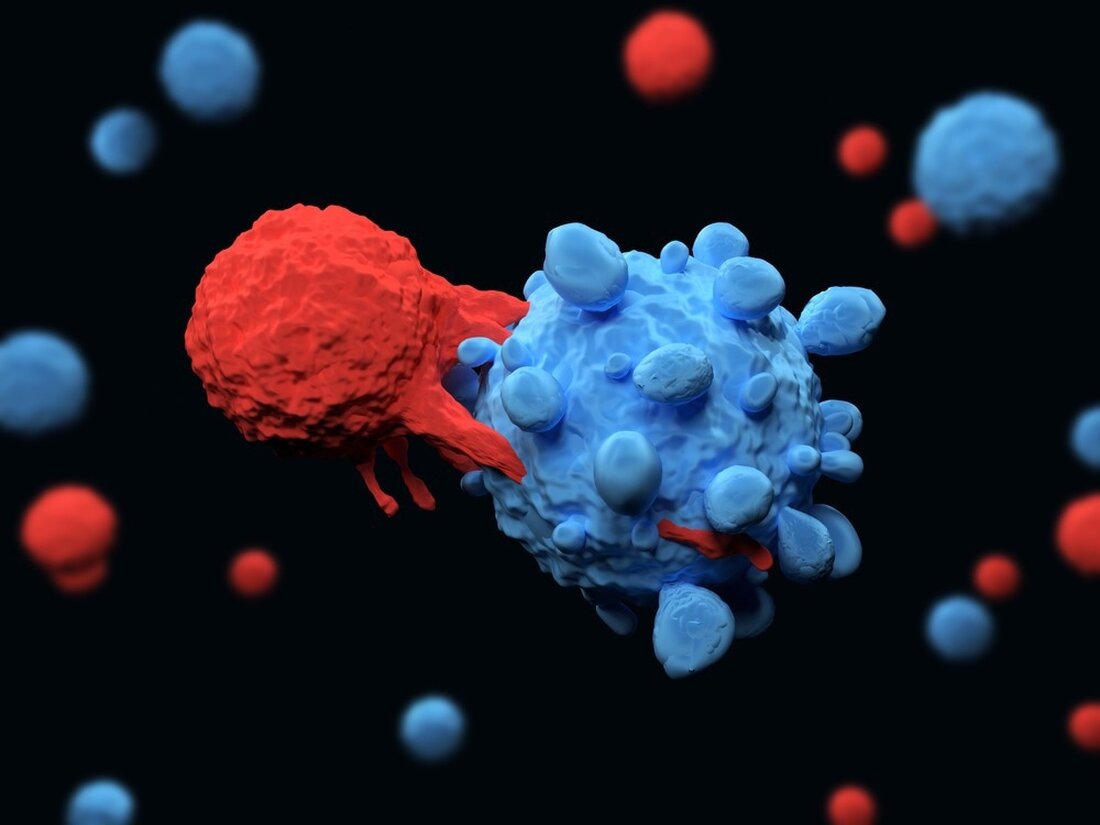
In a recently published study in Frontiers in Immunology, researchers examined the effectiveness of chimeric antigen receptor (CAR) T cells in immunotherapy for colorectal cancer (CRC). Learn: CAR T cells for colorectal cancer immunotherapy: Ready to go? Image credit: Meletios Verras/Shutterstock Background CAR-T cells are a novel cell-based immunotherapy against cancer that is genetically developed. The use of CAR T cells has transformed the treatment of hematological cancers. Extensive research is required before this therapy can be modified to treat solid tumors such as colon cancer. The treatment of colorectal cancer with CAR-T cells is still in its infancy and few clinical data are available. Among the significant disadvantages…
CAR T-cell therapy for colorectal cancer
In a recently published study in Frontiers in immunology Researchers examined the effectiveness of chimeric antigen receptor (CAR) T cells in immunotherapy for colorectal cancer (CRC).
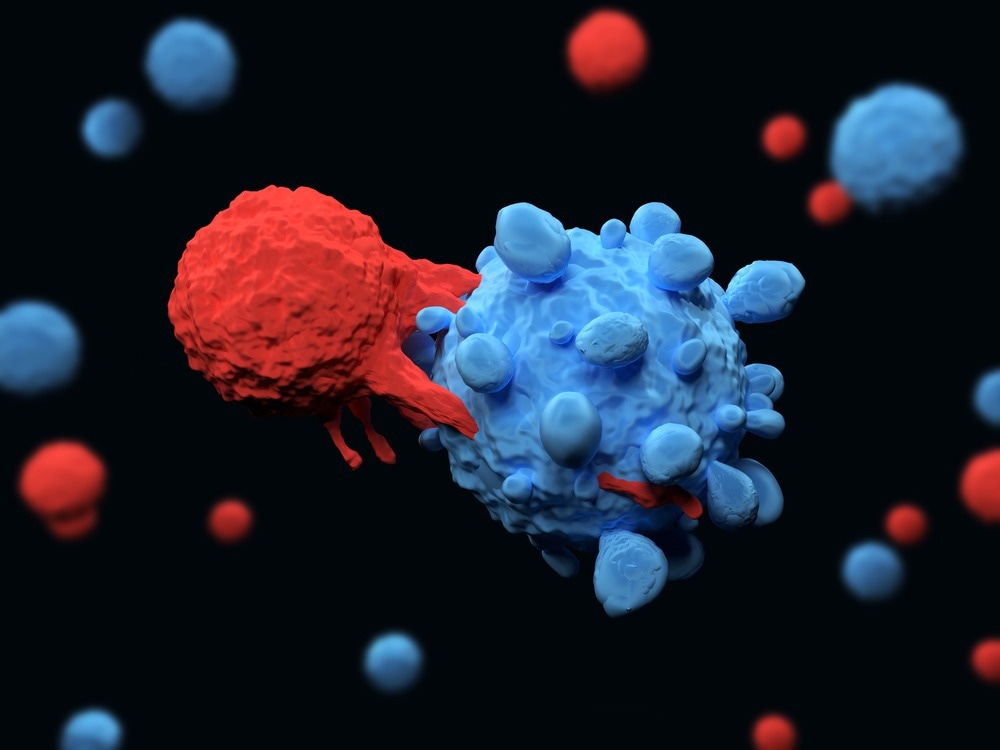
Lernen: CAR-T-Zellen für die Darmkrebs-Immuntherapie: Ready to go? Bildnachweis: Meletios Verras/Shutterstock
background
CAR-T cells are a novel cell-based immunotherapy against cancer that is genetically developed. The use of CAR T cells has transformed the treatment of hematological cancers. Extensive research is required before this therapy can be modified to treat solid tumors such as colon cancer. The treatment of colorectal cancer with CAR-T cells is still in its infancy and few clinical data are available. Significant drawbacks of CAR T-cell treatment of colorectal cancer include significant toxicity, relapse, and an impenetrable tumor microenvironment.
Biological features of CAR T cell engineering
In the present study, researchers evaluated CAR T-cell treatment for colorectal cancer in terms of existing knowledge, identified barriers, and future prospects.
CAR T-cell treatment is a personalized immunotherapy based on autologous or allogeneic, synthetic, genetically engineered CAR-expressing T cells. The CAR molecule consists of extracellular binding units, either a tumor-specific antigen (TSA) sensing element or a single-chain fragment derived from an antibody. There is also a transmembrane anchor in combination with signaling domains of the T cell receptor zeta chain complex and costimulatory molecules such as CD28 and 4-1BB.
Activation of CAR-T cells arises from the direct and specific identification of tumor antigens by the extracellular domain, resulting in the killing of cancer cells. A patient's T cells are typically transduced with gammaretroviral or lentiviral vectors to express CARs. After the ex vivo production of CAR T cells, lymphodepleting chemotherapy is carried out, if necessary with subsequent CAR T cell injection.
CAR T cells play a promising role in the treatment of CRC
First-line surgical and chemotherapy treatments for patients with CRC have long resulted in poor prognosis. Better understanding of the processes that contribute to tumor development and proliferation has enabled the development of targeted and effective drugs. Although CAR-T cells are excellent candidates against hematological malignancies, their effectiveness against solid tumors such as CRC remains unconfirmed. Several groups have focused on preclinical research on CAR T cell biology to establish safe treatment techniques and confirm their effectiveness in CRC.
Adhesion molecule for epithelial cells
One of the first preclinical investigations examined the lethal effects of epithelial cell adhesion molecules (EpCAM)-driven CAR-T cells. Normal epithelial cells express EpCAM, a transmembrane glycoprotein, on their surface. Its overexpression is associated with increased cell proliferation, invasion, migration and metastasis. Extensive peritoneal metastasis and ascites formation were observed in an in vivo immunodeficient mouse model of late-stage human metastatic cancer. Repeated injections of EpCAM-CAR-T cells inhibited the progression of peritoneal disease in xenotransplanted mice with tumors.
Carcinoembryonic antigen
E-Book Antibodies
Compilation of the top interviews, articles and news from the last year. Download a free copy
Carcinoembryonic antigen (CEA) is also a target of anti-CRC CAR T cells that have been explored. CEA is an immunoglobulin glycoprotein that is overexpressed in various human malignancies, including colon, lung, stomach, pancreatic, and ovarian cancers. CEA is one of the most important prognostic and diagnostic tumor indicators and is overexpressed in over 98% of CRC tissue samples. Therefore, CEA-targeted treatments have the potential to generate novel CRC therapeutic techniques. CAR-T cells targeting CEA have demonstrated excellent anticancer activity both in vitro and in vivo, which was significantly enhanced by the addition of interleukins such as interleukin (IL)-12.
Epidermal growth factor receptor
In a xenograft model created by coinoculating tumor cells with CAR-T cells, a study found that EGFRvIII CAR-T cells combined with miR-153 completely eradicated the tumor. These results suggested that miR-153 reduced indoleamine 2,3-dioxygenase (IDO)-1 expression in CRC cells and improved the efficacy of CAR-T cell treatment. Therefore, the combination of IDO1 inhibitors with CAR T cells has the potential to act as an effective treatment for CRC and solid tumors.
Studies have also found that engineered cells expressing a CAR capable of binding a fluorescein isothiocyanate (FITC) molecule (anti-FITC CAR T cells) improved the ability of CAR T cells to treat mice with estimated glomerular filtration rate (eGFR)-positive CRC tumors. In an immunocompromised mouse model, unique interactions between anti-FITC CAR T cells and FITC-labeled cetuximab slowed colon cancer progression.
CAR T-cell trials for CRC
Ongoing studies are investigating the use of CEA-specific CAR T cells in patients with CEA-positive CRC. The aim is to verify effectiveness and safety and to determine the correct doses and infusion schedules. Another aim of these studies is to identify undesirable effects, particularly cytokine release syndrome. Administration protocols include hepatic and systemic transarterial administration, vascular interventions, and intraperitoneal infusions while awaiting results.
Also being evaluated is a novel combinatorial technique involving human epidermal growth factor receptor 2 (HER2)-specific CAR-T cells together with an oncolytic adenovirus (CAdVEC). Oncolytic adenoviruses reproduce and multiply exclusively within tumors, increasing their cytotoxicity, enhancing tumor penetration, and reversing immunosuppression. CAdVEC is a modified adenovirus with immunostimulating components. Phase 1 trials are currently investigating the efficacy and safety of HER2-CAR-T cells in combination with oncolysis.
Conclusion
Overall, the study results showed that CAR-T cells continue to accumulate evidence supporting their use as a viable immunological method of cancer treatment. This strategy has significantly improved patient treatment for hematologic malignancies.
Reference:
- Ghazi, B. et al. (2022) „CAR T-cells for colorectal cancer immunotherapy: Ready to go?“, Frontiers in Immunology, 13. doi: 10.3389/fimmu.2022.978195. https://www.frontiersin.org/articles/10.3389/fimmu.2022.978195/full
.

 Suche
Suche
 Mein Konto
Mein Konto
