Immunological responses to monkeypox virus regarding the 2022 outbreak
Studies have reported more than 60,000 human cases of monkeypox in non-endemic countries as of May 2022. The current outbreak was observed to be different from previous monkeypox infections in Central and West Africa. This was due to the asynchronous development of the lesions as well as more frequent perianal and genital locations. This unusual monkeypox virus outbreak prompted the scientific community to discuss vaccination strategies for the high-risk groups, which mainly included men who have sex with men. Learning: Immunological signature in human monkeypox infection cases in 2022: an observational study. Image credit: Dotted Yeti/Shutterstock Background E-Book Immunology Compilation of the top interviews, articles and...

Immunological responses to monkeypox virus regarding the 2022 outbreak
Studies have reported more than 60,000 human cases of monkeypox in non-endemic countries as of May 2022. The current outbreak was observed to be different from previous monkeypox infections in Central and West Africa. This was due to the asynchronous development of the lesions as well as more frequent perianal and genital locations. This unusual monkeypox virus outbreak prompted the scientific community to discuss vaccination strategies for the high-risk groups, which mainly included men who have sex with men.
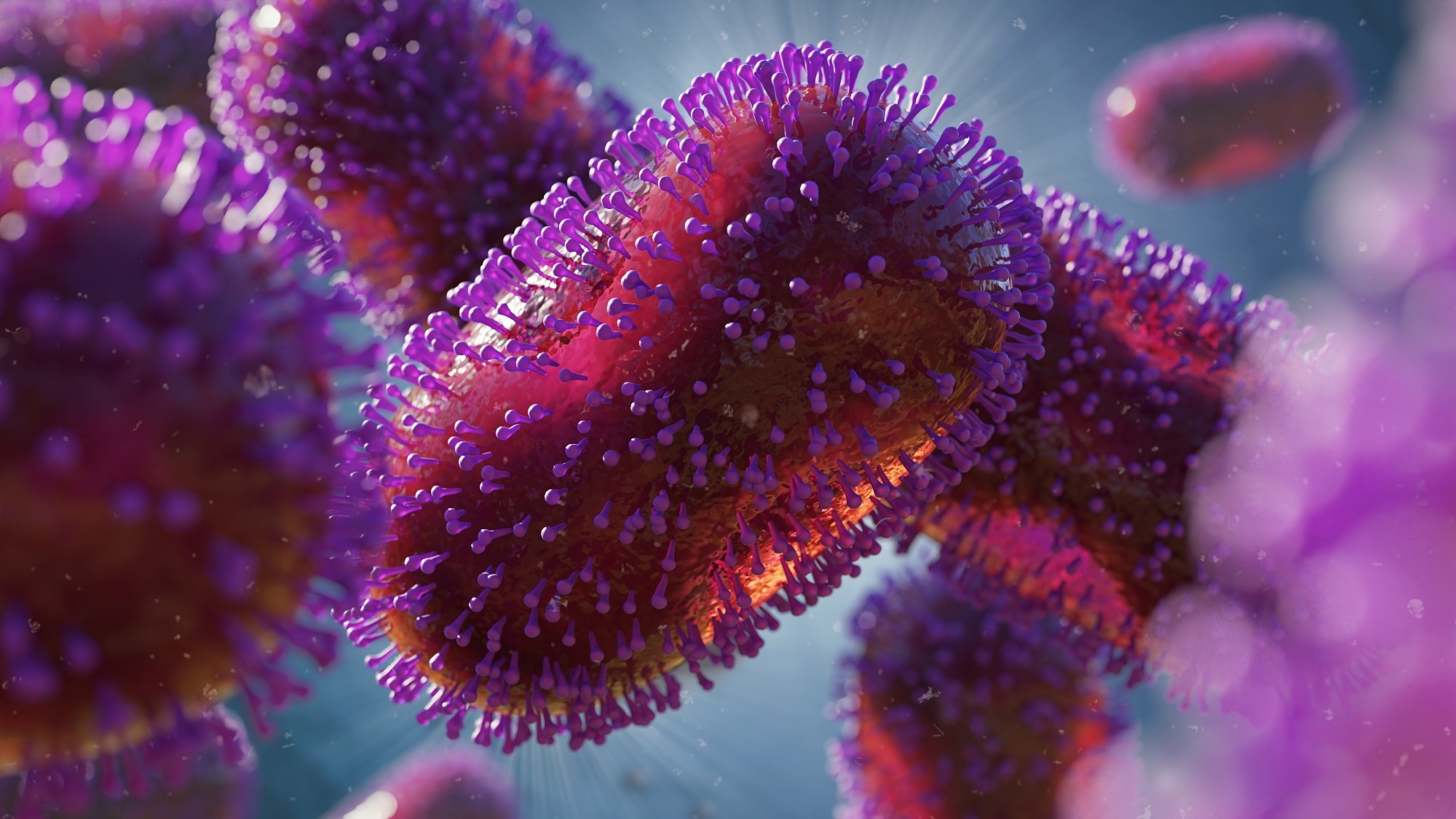
Lernen: Immunologische Signatur in Fällen einer Affenpockeninfektion beim Menschen im Jahr 2022: eine Beobachtungsstudie. Bildnachweis: Dotted Yeti/Shutterstock
background
Immunology e-book
Compilation of the top interviews, articles and news from the last year. Download a free copy
The smallpox vaccine has been reported to be 85% cross-protective against monkeypox virus. However, the restrictions include the restriction to people aged 40 and over and the controversial background immunity. The lack of protective immunity in young people can lead to the spread of the monkeypox virus among people.
Previous experiments in animal models suggest that all immune players help in viral clearance, with CD8+ T cells being the most important. In addition, one study reported that all recovery cases were positive for orthopoxvirus-specific IgG, IgM, B cell, and T cell responses. Additionally, an orthopoxvirus-specific immune response has been observed in some people who did not develop monkeypox infection.
It has been observed that smallpox vaccination cannot provide complete protection against the monkeypox virus, but it can protect against serious disease. In addition, overproduction of cytokines has been observed in patients with severe monkeypox infection, suggesting a relationship between clinical severity and an imbalanced immune response. However, no information is available on the dynamics of the immune response in humans during the current outbreak.
A new study published in The Lancet Infectious Diseases aimed to analyze the kinetics of smallpox-specific T cell induction, inflammatory profile, and inflammatory profile in human cases of the current monkeypox outbreak.
About studying
The study included 17 patients with laboratory-confirmed monkeypox virus positivity who were tested 10 to 12 days after symptom onset, as well as 10 healthy controls. Samples collected from all patients were divided into four groups: T0–T3, T4–T7, T8–T11, and T12–T20 days after symptom onset. Demographic, epidemiological, laboratory and clinical data were collected from all patients.
Flow cytometry was performed to analyze activation and differentiation of CD4+ and CD8+ T cells. Standard interferon-γ ELISpot was used to determine the frequency of T cell response to peptides from the modified vaccinia virus Ankara (MVA). Assessment of spontaneous cytokine production was performed by incubating peripheral blood mononuclear cells (PBMCs) collected from all participants on DMSO. An ELISA assay was performed to evaluate the production of cytokines after specific stimulation. Finally, quantification of IL-1β, IL-6, IL-8, and TNF in patient plasma was performed using automated multiplex immunoassays.
Study results
The results showed a mean age of the patients of 39.5 years. 7 were reported as HIV positive with antiretroviral therapy but undetectable HIV RNA and a CD4+ T cell count greater than 350 cells/µl. It was reported that the 10 HIV-negative participants received pre-exposure prophylaxis (PrEP). Sexual intercourse was reported as the route of transmission in 14 patients.
Systemic symptoms were observed in 14 patients, while those without systemic symptoms were considered paucisymptomatic. One patient had received a smallpox vaccination as a child and five were treated with antiviral drugs. The median recovery time was reported to be 15 days.
A lower percentage of CD4+ T cells and a higher percentage of CD8+ T cells were reported in patients shortly after infection compared to healthy controls. It was reported that six of nine monkeypox cases had lower frequencies of naïve CD4+ T cells than healthy controls. A lower proportion of naive and more terminally differentiated CD8+ T cells was observed in all patients. However, the proportion of CD4+ effector memory T cell frequencies was observed to be similar in patients and healthy controls after 12 to 20 days.
Higher CD4+CD38+ and CD8+CD38+ T cell frequencies were observed in patients compared to healthy controls, which were also similar for PD-1 and CD57 markers. No differences in immune cell profile were observed between HIV-positive and HIV-negative patients, while a less altered immune profile was observed in paucisymptomatic patients. Higher inflammatory cytokines (IL-1β, IL-6, IL-8 and TNF) were observed in monkeypox virus patients compared to controls, which remained higher even after recovery.
Furthermore, higher expression of CCR7, CD69, CXCR5, CD95, CCR6, CXCR3, CD28, CD4RA and CD27 was observed in patients compared to healthy controls in the post-acute phase. Similar results were observed for CD8+ T cells along with re-expression of CD45RA. Furthermore, patients with monkeypox showed a higher percentage of effector memory T cells that reexpressed CD45RA, that expressed CD57, PD1, or both.
Therefore, the current study demonstrated an early expansion of activated effector CD4+ and CD8+ T cells as a result of monkeypox virus infection that is sustained over time. All participants also developed a strong cytokine response regardless of HIV infection. Thus, the MVA vaccine can be used as an anti-monkeypox vaccine for the high-risk population. Further research on prolonged immunity is needed to support the current hypothesis.
restrictions
The study has certain limitations. First, data analyzing humoral response were not available. Second, only three poxvirus proteins were used as antigens. Third, the study does not involve a randomized selection of participants. Fourth, the number of participants was limited.
Reference:
- Agrati, C. et al. (2022). Immunologische Signatur in Fällen einer Affenpockeninfektion beim Menschen im Jahr 2022: eine Beobachtungsstudie. Die Lancet-Infektionskrankheiten. doi: https://doi.org/10.1016/S1473-3099(22)00662-4. https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(22)00662-4/fulltext.
.

 Suche
Suche
 Mein Konto
Mein Konto
