A clinical trial to evaluate an antiviral drug against monkeypox begins in the Democratic Republic of Congo
A clinical trial to evaluate the antiviral drug Tecovirimat, also known as TPOXX, in adults and children with monkeypox has begun in the Democratic Republic of Congo (DRC). The study will evaluate the safety of the drug and its ability to relieve symptoms of monkeypox and prevent serious consequences, including death. The National Institute of Allergy and Infectious Diseases (NIAID), part of the US National Institutes of Health, and the Democratic Republic of Congo's National Institute for Biomedical Research (INRB) are co-leading the study as part of the PALM Government-to-Government Partnership. The cooperating institutions include the US Centers for...
A clinical trial to evaluate an antiviral drug against monkeypox begins in the Democratic Republic of Congo
A clinical trial to evaluate the antiviral drug Tecovirimat, also known as TPOXX, in adults and children with monkeypox has begun in the Democratic Republic of Congo (DRC). The study will evaluate the safety of the drug and its ability to relieve symptoms of monkeypox and prevent serious consequences, including death. The National Institute of Allergy and Infectious Diseases (NIAID), part of the US National Institutes of Health, and the Democratic Republic of Congo's National Institute for Biomedical Research (INRB) are co-leading the study as part of the PALM Government-to-Government Partnership. The collaborating institutions include the US Centers for Disease Control and Prevention (CDC), the Antwerp Institute of Tropical Medicine, the aid organization Alliance for International Medical Action (ALIMA) and the World Health Organization (WHO).
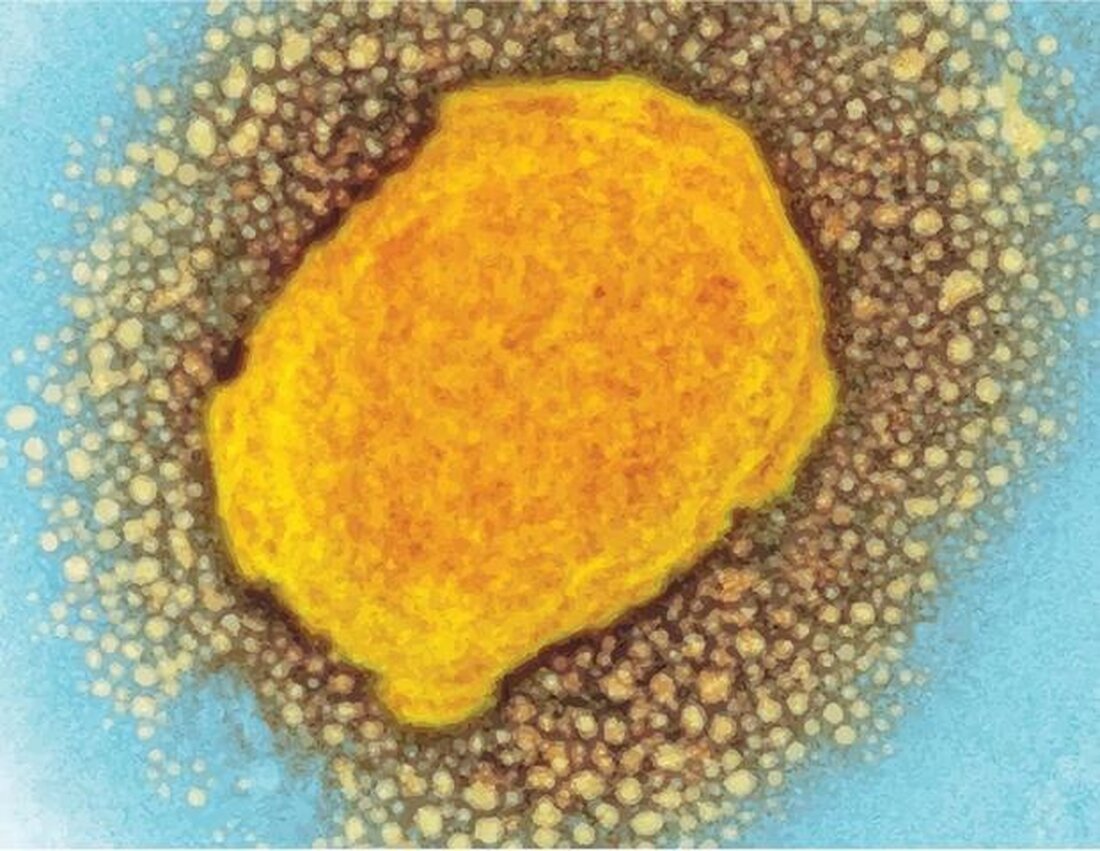
TPOXX, manufactured by the pharmaceutical company SIGA Technologies, Inc. (New York), is approved by the US Food and Drug Administration for the treatment of smallpox. The drug inhibits the spread of the virus in the body by preventing virus particles from escaping human cells. The drug targets a protein found on both the virus that causes smallpox and the monkeypox virus.
“Monkeypox has caused a high burden of disease and death in children and adults in the Democratic Republic of Congo, and improved treatment options are urgently needed,” said NIAID Director Anthony S. Fauci, MD. “This clinical trial will provide important information about this.” the safety and effectiveness of Tecovirimat in monkeypox. I would like to thank our scientific partners in the Democratic Republic of Congo and the Congolese people for their continued collaboration in advancing this important clinical research.”
Since the 1970s, the monkeypox virus has caused sporadic cases and outbreaks, primarily in the rainforest areas of Central Africa and West Africa. Since May 2022, there has been an outbreak of monkeypox on several continents in areas where the disease is not endemic, including Europe and the United States, with most cases occurring in men who have sex with men. The outbreak has led to recent public health emergency declarations by the WHO and the U.S. Department of Health and Human Services. From January 1, 2022 to October 5, 2022, WHO reported 68,900 confirmed cases and 25 deaths from 106 countries, areas and territories.
According to the WHO, cases identified in the ongoing global outbreak are largely caused by the monkeypox virus clade IIb. Group I is responsible for infections in the Democratic Republic of Congo and is estimated to cause more severe disease and higher mortality than groups IIa and IIb, particularly in children. The Africa Centers for Disease Control and Prevention (Africa CDC) reported 3,326 cases of monkeypox (165 confirmed; 3,161 suspected) and 120 deaths in the Democratic Republic of Congo from January 1, 2022 to September 21, 2022.
Humans can become infected with monkeypox through contact with infected animals such as rodents, nonhuman primates, or humans. The virus can be transmitted among people through direct contact with skin lesions, body fluids and respiratory droplets, including through intimate and sexual contact; and through indirect contact with contaminated clothing or bedding. Monkeypox can cause flu-like symptoms and painful skin lesions. Complications can include dehydration, bacterial infections, pneumonia, encephalitis, sepsis, eye infections and death.
The study will enroll up to 450 adults and children with a laboratory-confirmed monkeypox infection who weigh at least 3 kilograms (kg). Pregnant women are also eligible. Volunteer participants will be randomly assigned to receive either oral Tecovirimat or placebo capsules twice daily for 14 days, with the dose administered depending on the participant's weight. The study is double-blind, so participants and researchers do not know who is receiving tecovirimat or placebo.
All participants stay in a hospital for at least 14 days and receive supportive care there. Study physicians will monitor participants' clinical status regularly throughout the study and participants will be asked to provide blood, throat swab, and skin lesion swab samples for laboratory testing. The primary aim of the study is to compare the average time to healing of skin lesions in patients who received tecovirimat with those who received placebo. Researchers will also collect data on several secondary objectives, including comparisons of how quickly participants test negative for monkeypox virus in their blood, overall disease severity and duration, and mortality between groups.
Participants will be discharged from the hospital once all lesions have crusted or peeled off and after their blood tests negative for monkeypox virus for two consecutive days. You will be followed for at least 28 days and asked for an optional study visit after 58 days for further clinical and laboratory testing. An independent data and safety monitoring board will monitor the safety of participants throughout the duration of the study.
The study is led by co-principal investigators Jean-Jacques Muyembe-Tamfum, MD, Ph.D., Director General of the INRB and Professor of Microbiology at the Faculty of Medicine, Kinshasa University in Gombe, Kinshasa. and Placide Mbala, MD, Ph.D., operations manager of the PALM project and head of the Division of Epidemiology and the Pathogen Genomic Laboratory at INRB.
I am pleased that monkeypox is no longer a neglected disease and that thanks to this study we will soon be able to demonstrate that there is an effective treatment for this disease.”
Dr. Jean-Jacques Muyembe-Tamfum, MD, Ph.D., Director General of the INRB and Professor of Microbiology, University of Kinshasa Faculty of Medicine in Gombe, Kinshasa
For more information, visit Clinicaltrials.gov and search code NCT05559099. The testing period depends on the pace of enrollment. A separate NIAID-supported trial of TPOXX is currently underway in the United States. For information about the US study, visit the AIDS Clinical Trials Group (ACTG) website and search for TPOXX or study A5418.
PALM is short for “Pamoja Tulinde Maisha,” a Kiswahili phrase that translates to “Saving Lives Together.” NIAID and the DRC Ministry of Health established the PALM clinical research partnership in response to the Ebola outbreak in eastern DRC in 2018. The collaboration continued as a multilateral clinical research program composed of NIAID, the Ministry of Health of the Democratic Republic of Congo, INRB, and INRB's partners. PALM's first study was a multi-therapeutic randomized controlled trial for Ebola virus disease that supported regulatory approvals of the NIAID-developed treatments mAb114 (Ebanga) and REGN-EB3 (Inmazeb, developed by Regeneron).
Source:
.

 Suche
Suche
 Mein Konto
Mein Konto
