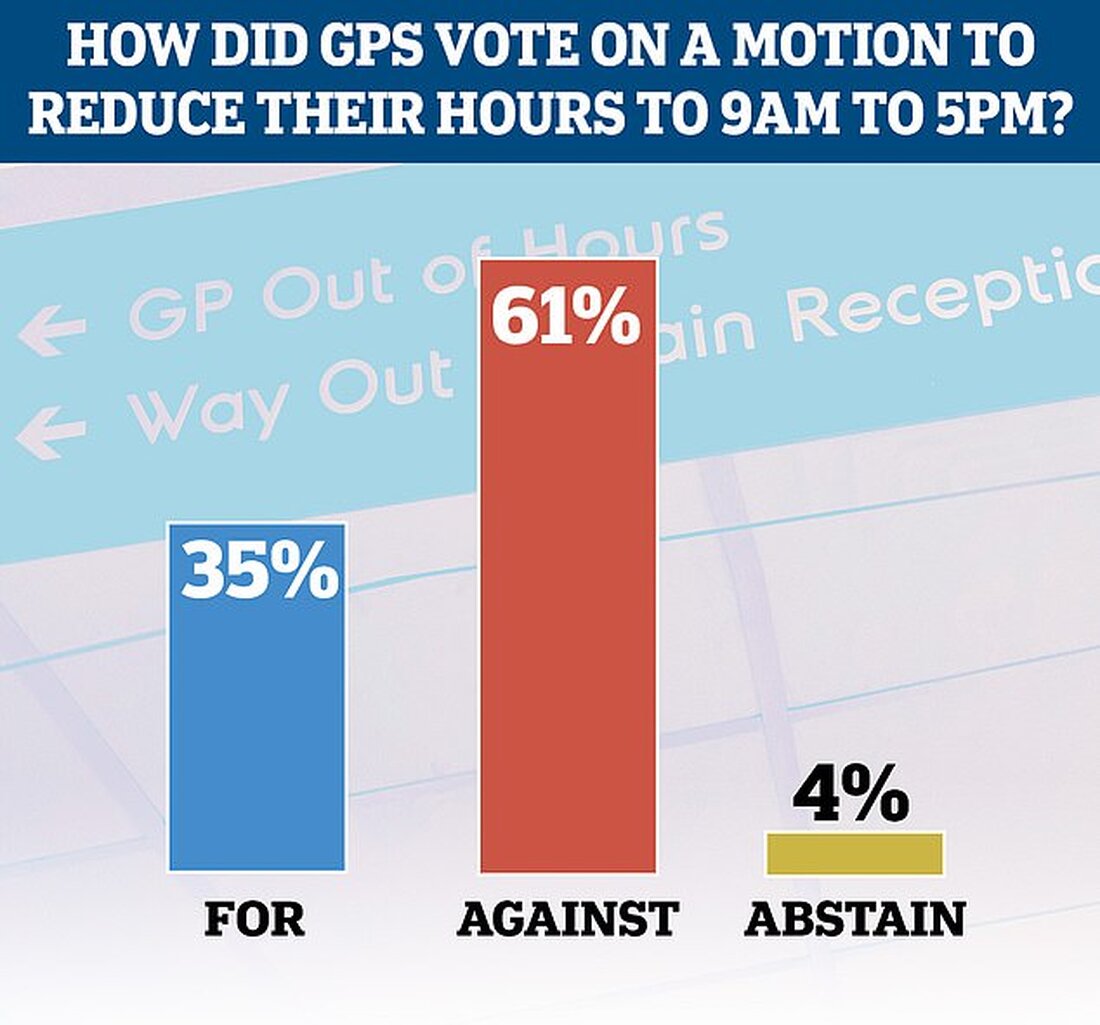
GPs have voted against a radical proposal to cut their consultation hours to 9am-5pm, but a shocking third backed the idea after a furious debate.
A proposal for GPs to cut their core hours from the current 8am to 6.30pm, Monday to Friday, sparked outrage last week as Brits continue to struggle to see their GPs.
While that motion failed, another British Medical Association (BMA) leader called for GP contracts to be renegotiated to address "inhumane" workload limits.
Both applications were submitted today at the annual conference of BMA local medical committee representatives in York.
As Dr. Shaba Nabi suggested the request for consultation, Dr. Shaba Nabi said there was pressure from other GPs to withdraw the application after being outraged by the idea last week, showing how "gaslit" the profession has been.
“Our working hours are completely at odds with any kind of family life - so we continue to bleed the GPs,” she said.
She said shortening opening hours would not deny patients access to care but would actually make it safer, with more GPs wanting to remain in work rather than seeking a better work-life balance.
Dr. However, LJ Evans urged her colleagues to reject the application as it would make the current situation worse.
“Patients are really struggling to see their GP, they are not happy, there are just not enough GP appointments,” she said.
“How on earth will reducing core GP hours help?”.
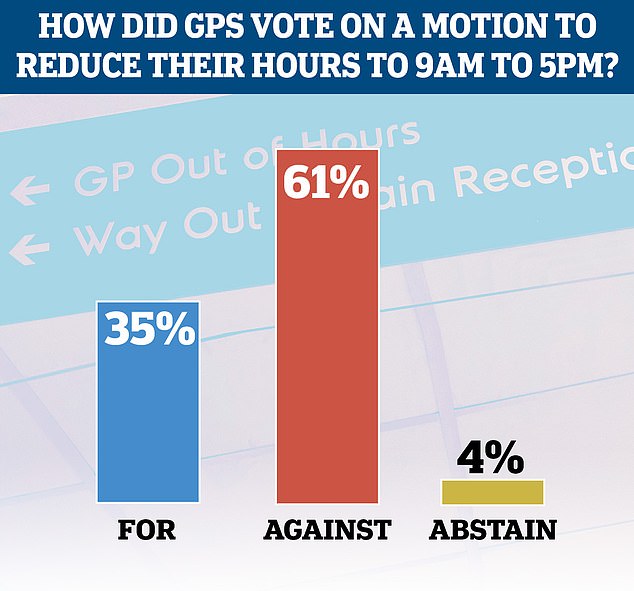
A controversial proposal for GPs to reduce their core hours to nine to five from the current 8am to 6.30pm was rejected today
As an out-of-hours GP, she also argued that practices that shorten their opening hours would only shift the problem of patients seeking help onto other medical professionals.
"We cover all the hours that the practices don't have. Do you think we don't have a workload-workplace mismatch?" she said.
“How can we find the extra 12.5 hours per week?”
After a heated debate, 61 percent of GPs voted against the motion, but shockingly more than a third supported it.
However, another motion calling on BMA leaders across the UK to “use safe workload data to renegotiate GMS contracts with workload limits to protect all general practice staff and patients” received their support.
Dr. Rachel McMahon, who tabled the motion, said the pressure being placed on GPs was “inhumane” and the expected workload was “unsustainable”.
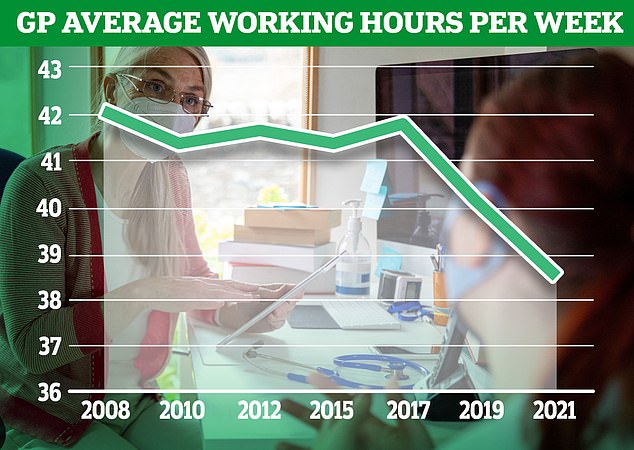
“Funding hasn’t kept up with demand and we’re working harder and harder,” she said.
Overall, 70 percent of GPs eligible to vote supported the motion, 24 percent opposed it, and the rest abstained.
Dennis Reed, the director of Silver Voices, a campaign group for the over-60s, told MailOnline he was "relieved" that the vote on the working time cuts had failed.
“This would be extremely bad publicity and unfair to many hard-working GPs who work beyond nine to five hours.”
"Core hours are not the big problem here. The big problem is that there is not sufficient coverage to ensure patient safety."
He said both the government and GPs needed to negotiate a more comprehensive solution to improve patient access to services, particularly in areas where patient-to-doctor ratios were high.
The debate over GP hours and patient access has raged since Britain emerged from lockdown and found some services, particularly face-to-face appointments with doctors, struggling to recover.
Just last month it was revealed that two-thirds of GP appointments in parts of England were not carried out by patients' actual doctors, according to the latest NSH data.
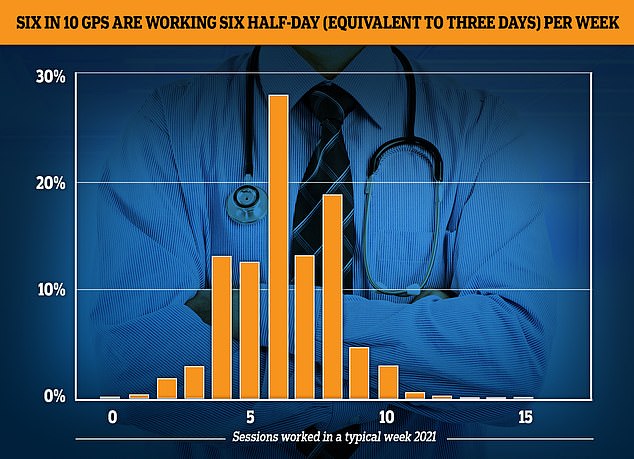
The GP Worklife survey found that more than half of GPs worked for six sessions a week or less each week in 2021, with each session lasting four hours and 10 minutes. Almost a fifth of the workforce saw patients for four sessions or less, while 12.4 percent worked for five sessions and 27.9 percent worked for six sessions
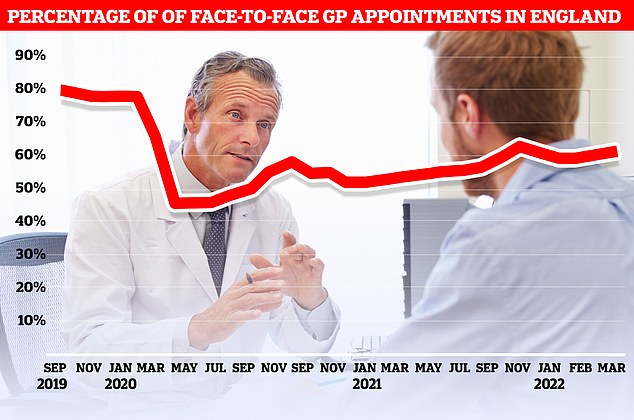
Only 62 percent of appointments were made in person last month. It was higher than the previous month (61 percent), but well below the more than 80 percent recorded in 2019
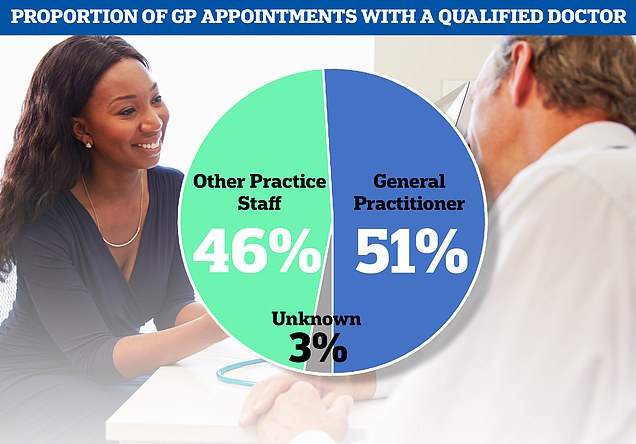
Overall, only 51 percent of patients in the country were seen by their primary care doctor. 46 percent were seen by other practice staff, including nurses, pharmacists and physiotherapists
NHS figures show just 36 per cent of patients were seen by a qualified GP in North East Lincolnshire in March, with the rest seen by other staff including nurses, physiotherapists or even acupuncturists.
In addition, only 62 percent of family doctor appointments in March were made in person.
While this was on theLast month (61 percent), it is well below the more than 80 percent of appointments that took place face-to-face before the pandemic.
And the figures also show that almost one in six appointments – whether with or without a family doctor – were over within five minutes.
DepartmentsBetween GPs and the public over the issue has been exacerbated by data showing almost six in 10 GPs, who earn an average of £100,000 a year, now work three days a week.

 Suche
Suche
 Mein Konto
Mein Konto