Two drugs not yet approved in the UK are the most effective drugs for treating insomnia, a major review has found.
Experts at the University of Oxford examined more than 150 studies testing the effects of 30 different medications on thousands of adults with sleep problems.
Eszopiclone, sold under the brand Lunesta, and lemborexant, marketed as Dayvigo, were best at relieving insomnia symptoms.
They worked better than benzodiazepines and Z-drugs, two powerful sleeping pills which NHS bosses want to phase out.
Both pills are already being used throughout Europe and the USA. They are hypnotics that calm the brain to put someone to sleep very quickly.
Study leader Professor Andrea Cipriani said he expected British regulators to consider approving both drugs given the results.
However, he noted that they can cause side effects such as headaches, dizziness and nausea - similar to addictive benzodiazepines.
Professor Cipriani said that non-pharmaceutical treatments such as: B. therapy should still be the treatment of first choice.


Researchers at the University of Oxford examined more than 150 studies testing the effects of 30 different medications on 44,000 adults with sleep problems. They found that eszopiclone, sold under the brand name Lunesta (left), and lemborexant, sold as Dayvigo (right), were best for relieving insomnia symptoms
Insomnia – defined as regular difficulty sleeping – is thought to affect up to one in ten people in Europe.
This can lead to reduced productivity, increased work absences and a higher risk of accidents.
Insomnia is also strongly linked to mental health disorders such as depression and alcohol addiction.
First-line treatment includes promoting “sleep hygiene,” simple methods such as going to bed at the same time every night, exercising, and limiting caffeine consumption before bed.
Some patients may be referred for cognitive behavioral therapy – a talk therapy that aims to manage problems by changing the way a person thinks. Brits can also be prescribed an app that offers a six-week self-help program.
General practitioners can also prescribe sleeping pills. However, this is rarely done because the drugs can cause serious side effects and dependence.
However, it is believed that 300,000 people in England are long-term users of Z-drugs and benzodiazepines.
Some take the medication for other reasons, such as anxiety.
Professor Cipriani said in a briefing for health and science journalists today that there was "little evidence" about how effective sleeping pills compare to each other.
This raises questions about whether doctors are “prescribing the right medications” to those who need them, she said.
Their study, published in The lancet reviewed 154 published and unpublished studies – completed by November 2021.
Experiments evaluated the tested effectiveness of 30 different insomnia medications in 44,089 adults with sleep disorders.
They examined patients who received medication for four weeks - as well as those who took medication for three months.
Three-quarters received a sleeping pill while one-quarter received a placebo drug.
The volunteers reported on their sleep quality, whether they stopped taking the pill and adverse events – such as dizziness, nausea, fatigue, headaches and sleepiness.
The results showed that eszopiclone and lemborexant outperformed other drugs.
A quarter of short-term eszopiclone users reported their symptoms improved, while 38 percent of those who took it for three months said they were able to sleep more easily.
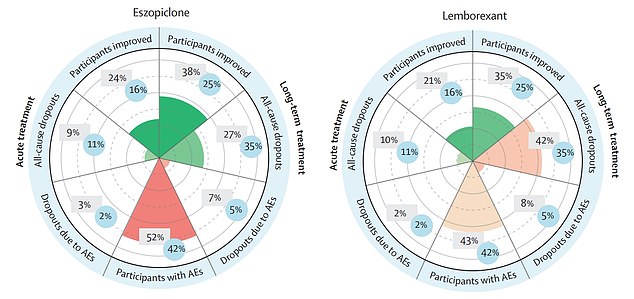
The graphic shows the effectiveness of eszopiclone (left) and lemborexant (right) for insomnia. A quarter of short-term eszopiclone users reported their symptoms improved, while 38 percent of those who took it for three months said they were able to sleep more easily. Meanwhile, one in five volunteers who took lemborexant said their symptoms improved after four weeks, while 35 percent said they subsided after three months. However, participants on both pills reported side effects
Meanwhile, one in five volunteers taking lemborexant said their symptoms had improved after four weeks, while 35 percent said they had subsided after three months.
However, researchers warned that up to half of patients treated with the two drugs felt unwell.
By comparison, benzodiazepines offered to patients in the UK were found to be effective in the short term - relieving up to three in 10 of users' symptoms.
However, researchers noted that no information is available about their long-term effects and patients do not tolerate them well, with up to six in ten reporting side effects.
Only 16 percent of patients benefited from Z-drugs such as Zaleplon and there was also a lack of long-term data.
And melatonin, another drug offered on the NHS, showed no significant benefits, with just 18 percent noticing an improvement and four in 10 reporting side effects, the team said.
The researchers said the safety data on lemborexant were inconclusive, but there appeared to be a risk of headaches, while users of eszopiclone reported dizziness and nausea.
More studies are needed to determine how safe the two drugs are over time, researchers said.
Professor Cipriani, a psychiatrist at the University of Oxford, said the results were “the most transparent and comprehensive picture of all the data available” on sleeping pills.
He said the results could help doctors identify the most appropriate drug for their insomnia patients and said regulators should consider the results when deciding whether to approve eszopiclone and lemborexant.
“The need to treat insomnia as effectively as possible is clearly very important as it can have an impact on a patient's health, their personal life and the wider healthcare system,” Professor Cipriani said.
However, he cautioned that the study "is not a recommendation that medication should always be used as a first line of support to treat insomnia" and warned that some could have "serious side effects."
However, Professor Cipriani noted that research shows that some drugs “can also be effective and should be used in clinical practice where appropriate”.
“For example, if treatments such as improved sleep hygiene and CBT have not worked, or if a patient wants to consider taking medication as part of their treatment,” he added.

 Suche
Suche
 Mein Konto
Mein Konto

