Brain AVM (arteriovenous malformation)
Brain AVM (arteriovenous malformation)
overview
Brain AVM
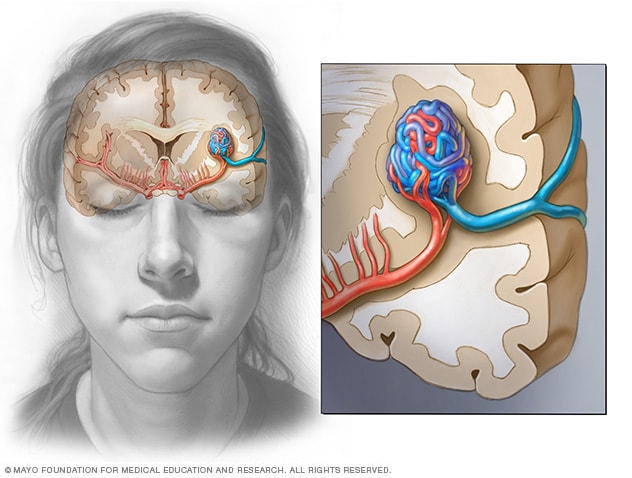
Brain AVM
In a brain AVM, blood flows directly from the arteries to the veins via tortuous vessels. This disrupts the typical process of how blood circulates through the brain.
Blood vessels in the brain AVM
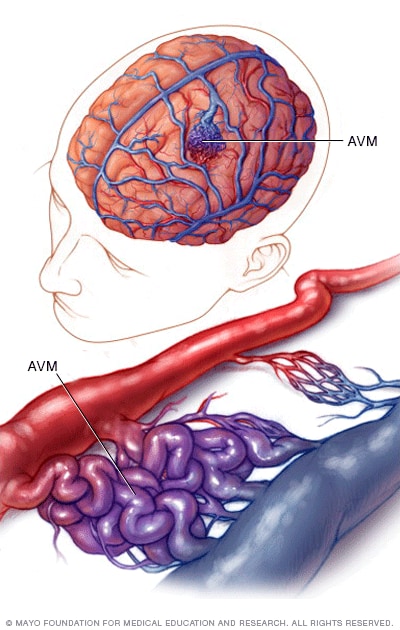
Blood vessels in the brain AVM
In an arteriovenous malformation of the brain, blood flows directly from the arteries to the veins through a tangle of blood vessels.
A brain arteriovenous malformation (AVM) is a tangle of blood vessels that connects arteries and veins in the brain.
The arteries carry oxygen-rich blood from the heart to the brain. Veins carry deoxygenated blood back to the lungs and heart. A brain AVM disrupts this vital process.
An arteriovenous malformation can develop anywhere in the body, but common locations include the brain and spinal cord - although AVMs in the brain are rare overall.
The cause of brain AVMs is not clear. Most people are born with them, but they can form later in life. Rarely they can be passed down within the family.
Some people with AVMs in the brain experience signs and symptoms such as headaches or seizures. An AVM is often found after a brain scan for another health problem or after blood vessels rupture and bleed (hemorrhage).
Once diagnosed, a brain AVM can be treated to prevent complications such as brain damage or stroke.
Symptoms
A brain arteriovenous malformation may not cause any signs or symptoms until the AVM ruptures, leading to bleeding. In about half of all brain AVMs, bleeding is the first sign.
But some people with brain AVMs may have signs and symptoms other than bleeding, such as:
- Krampfanfälle
- Kopfschmerzen oder Schmerzen in einem Bereich des Kopfes
- Muskelschwäche oder Taubheit in einem Teil des Körpers
Some people may experience more severe neurological signs and symptoms depending on the location of the AVM, including:
- Starke Kopfschmerzen
- Schwäche, Taubheit oder Lähmung
- Sehkraftverlust
- Schwierigkeiten beim Sprechen
- Verwirrung oder Unfähigkeit, andere zu verstehen
- Starke Unsicherheit
Signs and symptoms of a brain AVM can begin at any age, but usually appear between the ages of 10 and 40. Brain AVMs can damage brain tissue over time. The effects build up slowly and often cause symptoms in early adulthood.
However, in middle age, AVMs in the brain tend to remain stable and are less likely to cause symptoms.
Research has not found that pregnancy increases the risk of bleeding for people with a brain AVM. However, more research needs to be done.
A severe type of brain AVM affects the vein of Galen. It causes signs and symptoms that appear shortly or immediately after birth. The large blood vessel involved in this type of brain AVM can cause fluid to build up in the brain and the head to swell. It can also cause swollen veins visible on the scalp, seizures, failure to thrive, and congestive heart failure.
When to go to the doctor?
Seek immediate medical attention if you notice any signs or symptoms of a brain AVM, such as: B. Seizures, headaches or other symptoms. A bleeding brain AVM is life-threatening and requires emergency medical care.
Causes
AVM blood flow
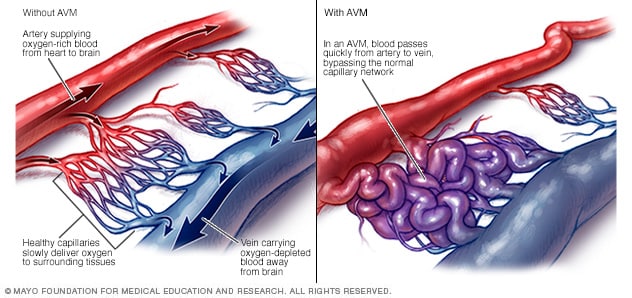
AVM blood flow
An arteriovenous malformation (AVM) causes blood to flow rapidly from the arteries to the veins, disrupting typical blood flow and supplying oxygen to surrounding tissues.
The cause of brain AVM is unknown. Researchers believe that most brain AVMs are present at birth and form during fetal development, but brain AVMs can also develop later in life. Brain AVMs are seen in some people with hereditary hemorrhagic telangiectasia (HHT), also known as Osler-Weber-Rendu syndrome. HHT affects the way blood vessels form in several areas of the body, including the brain.
Typically, the heart sends oxygen-rich blood to the brain through arteries. The arteries slow blood flow by directing it through a series of increasingly smaller networks of blood vessels, ending in the smallest blood vessels (capillaries). The capillaries slowly deliver oxygen to the surrounding brain tissue through their thin, porous walls.
The deoxygenated blood enters small blood vessels and then larger veins, which return the blood to the heart and lungs for more oxygen.
The arteries and veins in an AVM lack this supportive network of smaller blood vessels and capillaries. Instead, blood flows quickly and directly from the arteries to the veins, bypassing the surrounding tissues.
Risk factors
Anyone can be born with a brain AVM, but these factors can increase the risk:
- Männlich sein. Gehirn-AVMs sind häufiger bei Männern.
- Eine Familiengeschichte haben. In seltenen Fällen wurde berichtet, dass Gehirn-AVMs in Familien auftreten, aber es ist unklar, ob es einen bestimmten genetischen Faktor gibt oder ob die Fälle nur zufällig sind. Es ist auch möglich, andere Erkrankungen zu erben, die das Risiko von Hirn-AVMs erhöhen, wie z. B. erbliche hämorrhagische Teleangiektasie (HHT).
Complications
Cerebral hemorrhage
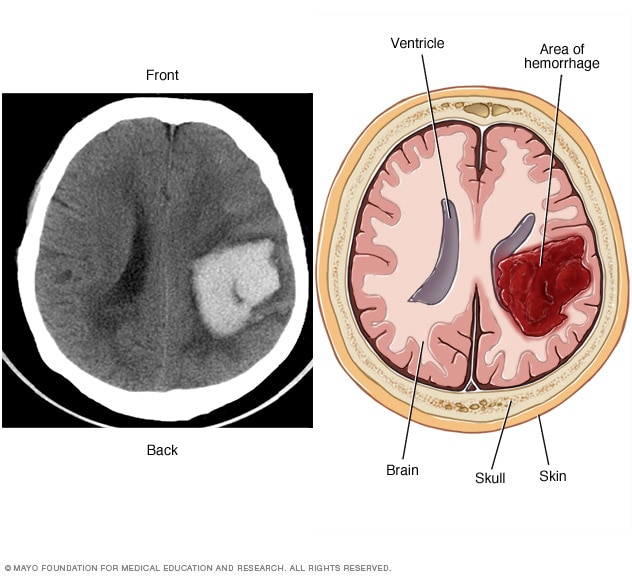
Cerebral hemorrhage
A brain AVM can cause bleeding in the brain (hemorrhage), which can damage surrounding brain tissue, as shown in this CT scan (left) and image (right) of an intracerebral hemorrhage.
Complications of a brain AVM include:
-
Bleeding in the brain.An AVM puts extreme pressure on the walls of affected arteries and veins, causing them to become thin or weak. This can cause the AVM to rupture and bleed into the brain.
This risk of AVM cerebral hemorrhage ranges between approximately 2% and 3% each year. The risk of bleeding may be higher with certain types of AVM or with a previous AVM rupture.
Some AVM-related bleeds go undetected because they do not cause major brain damage or signs or symptoms. However, potentially life-threatening bleeding episodes can occur.
Brain AVMs account for approximately 2% of all hemorrhagic strokes each year. They are often the cause of bleeding in children and young adults who suffer a cerebral hemorrhage.
-
Reduced oxygen to brain tissue.In a brain AVM, blood bypasses the network of capillaries and flows directly from the arteries to the veins. The blood flows quickly through the changed path because it is not slowed down by channels of smaller blood vessels.
Surrounding brain tissue cannot easily absorb oxygen from the fast-flowing blood. Without enough oxygen, brain tissue weakens or may die completely. This leads to stroke-like symptoms such as difficulty speaking, weakness, numbness, loss of vision or severe unsteadiness.
- Dünne oder schwache Blutgefäße. Eine AVM übt extremen Druck auf die dünnen und schwachen Wände der Blutgefäße aus. Eine Ausbuchtung in einer Blutgefäßwand (Aneurysma) kann sich entwickeln und anfällig für Ruptur werden.
-
Brain damage.The body can recruit more arteries to supply blood to the fast-flowing brain AVM. As a result, some AVMs can grow larger and displace or compress parts of the brain. This can prevent protective fluids from flowing freely around the brain hemispheres.
When fluid builds up, it can push brain tissue against the skull.
AVM (arteriovenous malformation) treatment of the brain
Sources:
- Informationsseite zu arteriovenösen Fehlbildungen. Nationales Institut für neurologische Erkrankungen und Schlaganfälle. https://www.ninds.nih.gov/Disorders/All-Disorders/Arteriovenous-Malformation-Information-Page. Abgerufen am 16. Dezember 2021.
- Was ist eine arteriovenöse Fehlbildung. American Stroke Association. https://www.stroke.org/en/about-stroke/types-of-stroke/hemorrhagic-strokes-bleeds/what-is-an-arteriovenous-malformation. Abgerufen am 16. Dezember 2021.
- Sänger RJ, et al. Arteriovenöse Missbildungen des Gehirns. https://www.uptodate.com/contents/search. Abgerufen am 16. Dezember 2021.
- Merkblatt zu neurologischen diagnostischen Tests und Verfahren. Nationales Institut für neurologische Erkrankungen und Schlaganfälle. https://www.ninds.nih.gov/Disorders/Patient-Cargiver-Education/Fact-Sheets/Neurological-Diagnostic-Tests-and-Procedures-Fact. Abgerufen am 16. Dezember 2021.
- Chen CJ, et al. Arteriovenöse Missbildungen des Gehirns. Neurologie. 2020; doi:10.1212/WNL.0000000000010968.
- Shaligram SS, et al. Risikofaktoren für Blutungen bei arteriovenösen Fehlbildungen des Gehirns. ZNS Neurowissenschaft und Therapeutik. 2019; doi:10.1111/cns.13200.
- Rutledge C, et al. Arteriovenöse Missbildungen des Gehirns. Handbuch der klinischen Neurologie. 2021; doi:10.1016/B978-0-444-64034-5.00020-1.
- Stimmungsstörungen nach Schlaganfall. American Stroke Association. https://www.stroke.org/en/about-stroke/effects-of-stroke/emotional-effects-of-stroke/post-stroke-mood-disorders. Abgerufen am 16. Dezember 2021.
- Fragen Sie MayoExpert. Hirngefäßfehlbildungen. Mayo-Klinik; 2021.
- Ferri FF. AV-Fehlbildungen, zerebral. In: Ferri’s Clinical Advisor 2022. Elsevier; 2022. https://www.clinicalkey.com. Abgerufen am 17. Dezember 2021.
- Davidoff CL, et al. Risiko der ersten Blutung von arteriovenösen Fehlbildungen des Gehirns während der Schwangerschaft: Eine systematische Überprüfung der Literatur. Neurochirurgie. 2019; doi:10.1093/neuros/nyz175.
- Merkblatt Arteriovenöse Fehlbildungen und andere vaskuläre Läsionen des zentralen Nervensystems. Nationales Institut für neurologische Erkrankungen und Schlaganfälle. https://www.ninds.nih.gov/Disorders/Patient-Cargiver-Education/Fact-Sheets/Arteriovenous-Malformation-Fact-Sheet. Abgerufen am 30. Dezember 2021.
- Ye X, et al. Ein dreidimensionales, farbgedrucktes System, das die vollständige Modellierung arteriovenöser Fehlbildungen für chirurgische Simulationen ermöglicht. Zeitschrift für klinische Neurowissenschaften. 2020; doi:10.1016/j.jocn.2020.04.123.
- Soldozy S. et al. Systematische Überprüfung der funktionellen Kartierung und kortikalen Reorganisation bei arteriovenösen Fehlbildungen, die anatomische Eloquenz neu definieren. Grenzen in der Chirurgie. 2020; doi:10.3389/fsurg.2020.514247.
- Ami T. Allscripts EPSi. Mayo-Klinik. 5. Januar 2022.

 Suche
Suche
 Mein Konto
Mein Konto