Leukoplakia
Leukoplakia
overview
Leukoplakia
Leukoplakia
Leukoplakia appears as thick, white patches on the inside of your mouth. It has a number of possible causes, including repeated injury or irritation. It can also be a sign of precancerous changes in the mouth or oral cancer.
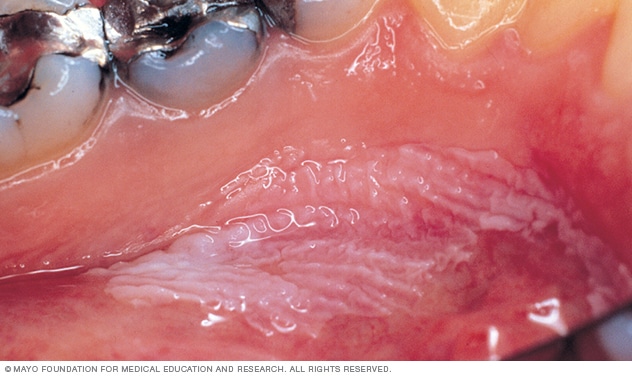
In leukoplakia (loo-koh-PLAY-key-uh), thickened, white patches form on your gums, the insides of your cheeks, the bottom of your mouth, and sometimes on your tongue. These patches cannot be scratched off.
Doctors don't know what causes leukoplakia, but consider chronic irritation from tobacco - whether smoked, dipped or chewed - as the main cause of its development.
Most leukoplakia spots are benign (benign), although some show early signs of cancer. Cancer of the floor of the mouth may occur adjacent to areas of leukoplakia. And white areas mixed with red areas (mottled leukoplakia) may indicate the potential for cancer. It is therefore best to see your dentist or family doctor if you have any unusual, persistent changes in your mouth.
A type of leukoplakia called hairy leukoplakia, sometimes called oral hairy leukoplakia, primarily affects people whose immune systems have been weakened by disease, particularly HIV/AIDS.
Symptoms
Leukoplakia usually occurs on your gums, the insides of your cheeks, the bottom of your mouth - under the tongue - and sometimes your tongue. It is usually not painful and may go unnoticed for a while.
Leukoplakia can occur:
- Weiße oder gräuliche Flecken, die nicht weggewischt werden können
- Unregelmäßig oder flach strukturiert
- Stellenweise verdickt oder verhärtet
- Zusammen mit erhabenen, roten Läsionen (gesprenkelte Leukoplakie oder Erythroplakie), die eher präkanzeröse Veränderungen zeigen
Hairy leukoplakia
Hairy leukoplakia causes fuzzy, white patches that resemble wrinkles or ridges, usually on the sides of your tongue. It is often confused with oral thrush, an infection characterized by creamy white patches that can be wiped away, which is also common in people with weakened immune systems.
When to go to the doctor?
Although leukoplakia usually causes no symptoms, it can sometimes indicate a more serious condition.
Contact your dentist or family doctor if you have any of the following problems:
- Weiße Plaques oder wunde Stellen im Mund, die nicht innerhalb von zwei Wochen von selbst abheilen
- Klumpen oder weiße, rote oder dunkle Flecken im Mund
- Anhaltende Veränderungen im Gewebe Ihres Mundes
- Ohrenschmerzen beim Schlucken
- Fortschreitende Verringerung der Fähigkeit, Ihren Kiefer zu öffnen
Causes
Although the cause of leukoplakia is unknown, chronic irritation, such as from tobacco use, including smoking and chewing, appears to be responsible for most cases. Often, regular users of smokeless tobacco products end up developing leukoplakia when they hold the tobacco to their cheeks.
Other causes may include chronic irritation caused by:
- Gezackte, gebrochene oder scharfe Zähne, die auf der Zungenoberfläche reiben
- Kaputte oder schlecht sitzende Prothesen
- Langfristiger Alkoholkonsum
Your dentist can talk to you about what might be causing leukoplakia in your case.
Hairy leukoplakia
Hairy leukoplakia is caused by an infection with the Epstein-Barr virus (EBV). Once you are infected with EBV, the virus remains in your body for life. Normally the virus is dormant, but if your immune system is weakened, particularly by HIV/AIDS, the virus can reactivate, leading to conditions such as hairy leukoplakia.
Risk factors
Tobacco use, especially smokeless tobacco, puts you at high risk for leukoplakia and oral cancer. Long-term alcohol consumption increases your risk, and alcohol consumption combined with smoking increases your risk even more.
Hairy leukoplakia
People with HIV/AIDS are particularly likely to develop hairy leukoplakia. Although the use of antiretroviral drugs has reduced the number of cases, hairy leukoplakia still affects a number of HIV-positive people and may be one of the first signs of HIV infection.
Complications
Leukoplakia usually doesn't cause permanent damage to the tissues in your mouth. However, leukoplakia increases your risk of oral cancer. Oral cancer often forms near leukoplakia spots, and the spots themselves may show cancerous changes. Even after the leukoplakia patches are removed, the risk of oral cancer remains.
Hairy leukoplakia
Hairy leukoplakia is unlikely to lead to cancer. But it may indicate HIV/AIDS.
prevention
You may be able to prevent leukoplakia if you avoid all tobacco products or alcohol consumption. Talk to your doctor about methods to help you quit. If you continue to smoke, chew tobacco, or drink alcohol, see your dentist regularly. Oral cancer is usually painless until it is fairly advanced, so avoiding tobacco and alcohol is a better prevention strategy.
Hairy leukoplakia
If you have a weakened immune system, you may not be able to prevent hairy leukoplakia, but early detection can help you receive appropriate treatment.
Sources:
- Leukoplakie. Informationszentrum für genetische und seltene Krankheiten. https://rarediseases.info.nih.gov/diseases/6897/leukoplakie. Abgerufen am 10. April 2017.
- Goldstein BG, et al. Läsionen im Mund. http://www.uptodate.com/home. Abgerufen am 10. April 2017.
- Sullivan JL. Klinische Manifestationen und Behandlung der Epstein-Barr-Virusinfektion. http://www.uptodate.com/home. Abgerufen am 10. April 2017.
- Lodi G., et al. Interventionen zur Behandlung von oraler Leukoplakie zur Vorbeugung von Mundkrebs (Review). Cochrane-Datenbank für systemische Reviews. http://ovidsp.tx.ovid.com/sp-3.24.1b/ovidweb.cgi?&S=OEPBFPAAJJDDEBDJNCHKEEOBALIJAA00&Link+Set=S.sh.19%7c4%7csl_50. Abgerufen am 10. April 2017.
- Kayalvizhi EB, et al. Orale Leukoplakie: Eine Überprüfung und ihre Aktualisierung. Zeitschrift für Medizin, Radiologie, Pathologie und Chirurgie. 2016;2:18.
- Saxena A. et al. Leukoplakie: Die Warzenarten. Internationale Zeitschrift für Stomatologie und Okklusionsmedizin. 2016;8:S10.
- Mundkrebs erkennen: Ein Leitfaden für medizinisches Fachpersonal. Nationales Institut für zahnärztliche und kraniofaziale Forschung. https://www.nidcr.nih.gov/OralHealth/Topics/OralCancer/DetectingOralCancer.htm#. Abgerufen am 12. April 2017.
- Salinas TJ (Gutachten). Mayo Clinic, Rochester, Minnesota, 18. April 2017.

 Suche
Suche
 Mein Konto
Mein Konto