anthrax
anthrax
overview
Anthrax is a rare but serious disease caused by a spore-forming bacteria, Bacillus anthracis. Anthrax primarily affects livestock and game. People can become infected through direct or indirect contact with sick animals.
There is no evidence that anthrax is transmitted from person to person, but it is possible that anthrax skin lesions are contagious through direct contact or through contact with a contaminated object (fomite). Anthrax bacteria usually enter the body through a wound in the skin. You can also become infected by eating contaminated meat or inhaling the spores.
Signs and symptoms, depending on how you are infected, may include skin sores, vomiting, and shock. Prompt treatment with antibiotics can cure most anthrax infections. Inhaled anthrax is more difficult to treat and can be fatal.
Anthrax is very rare in industrialized countries. However, the disease remains a concern because the bacteria have been used in bioterrorism attacks in the United States.
Symptoms
There are four common routes of anthrax infection, each with different signs and symptoms. In most cases, symptoms develop within six days of exposure to the bacteria. However, it is possible that it may take longer than six weeks for symptoms of inhalation anthrax to appear.
Cutaneous anthrax
Cutaneous anthrax

Cutaneous anthrax
You can get anthrax if spores get into your skin, usually through an open wound. The infection begins with a raised, sometimes itchy bump that resembles an insect bite. But within a day or two, the bump develops into an open, usually painless sore with a black center.
A skin-related (cutaneous) anthrax infection enters your body through the skin, usually through a cut or other wound. It is by far the most common route of the disease. It is also the mildest. With appropriate treatment, cutaneous anthrax is rarely fatal. Signs and symptoms include:
- Eine erhabene, juckende Beule, die einem Insektenstich ähnelt und sich schnell zu einer schmerzlosen Wunde mit einem schwarzen Zentrum entwickelt
- Schwellung in der Wunde und in der Nähe von Lymphdrüsen
- Manchmal grippeähnliche Symptome wie Fieber und Kopfschmerzen
Gastrointestinal anthrax
Gastrointestinal anthrax infection occurs from eating undercooked meat from an infected animal. It can affect your gastrointestinal tract from your throat to your colon. Signs and symptoms include:
- Brechreiz
- Erbrechen
- Bauchschmerzen
- Kopfschmerzen
- Appetitverlust
- Fieber
- Schwere, blutige Durchfälle in den späteren Stadien der Krankheit
- Halsschmerzen und Schluckbeschwerden
- Geschwollener Hals
Anthrax when inhaled
Anthrax when inhaled
Anthrax when inhaled
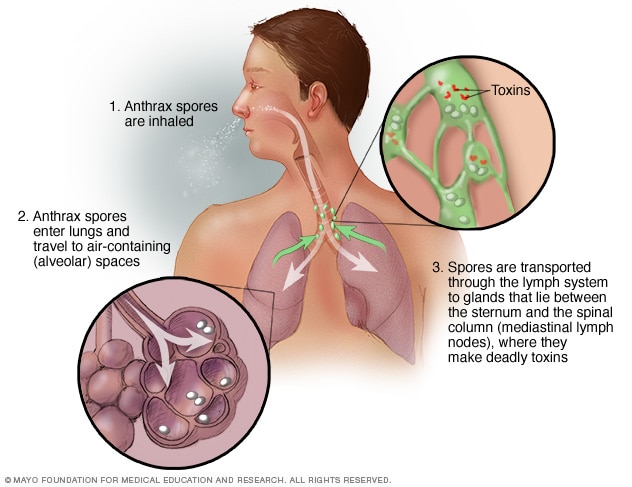
This illustration shows how the spores that cause inhalational anthrax - the deadliest form of anthrax infection - enter and affect the body.
Inhalational anthrax occurs when you inhale anthrax spores. It is the deadliest form of the disease and is often fatal even with treatment. The first signs and symptoms are:
- Grippeähnliche Symptome für einige Stunden oder Tage, wie Halsschmerzen, leichtes Fieber, Müdigkeit und Muskelschmerzen
- Leichte Brustbeschwerden
- Kurzatmigkeit
- Brechreiz
- Blut husten
- Schmerzhaftes Schlucken
- Hohes Fieber
- Atembeschwerden
- Schock – ein akuter medizinischer Zustand mit Zusammenbruch des Kreislaufsystems
- Meningitis
Injected anthrax
This recently identified anthrax infection route has previously only been reported in Europe. It is transmitted by injecting illegal drugs. The first signs and symptoms are:
- Rötung im Bereich der Injektion (ohne Bereich, der sich schwarz ändert)
- Deutliche Schwellung
- Schock
- Multiples Organversagen
- Meningitis
When to go to the doctor?
Many common illnesses begin with flu-like symptoms. The chances that your sore throat and muscle pain are due to anthrax are extremely small.
If you think you may have been exposed - for example, if you work in an environment where anthrax is likely to occur - seek immediate medical attention for evaluation and treatment. If you develop signs and symptoms of the disease after contact with animals or animal products in parts of the world where anthrax is common, seek medical attention immediately. Early diagnosis and treatment are crucial.
Causes
Anthrax spores are produced by anthrax bacteria, which occur naturally in soil in most parts of the world. The spores can lie dormant for years until they find their way into a host. Common hosts for anthrax are wild or farm animals such as sheep, cattle, horses and goats.
Although rare in the United States, anthrax is still common in the developing world, in countries such as Central America and South America, Sub-Saharan Africa, Central Asia and Southwest Asia, Southern Europe and Eastern Europe, and the Caribbean.
Most cases of anthrax in humans occur as a result of contact with infected animals or their meat or hides. In the United States, some people developed anthrax while making traditional African drums from the skins of infected animals.
One of the few known cases of non-animal transmission was a bioterrorism attack in the United States in 2001. Twenty-two people became ill with anthrax after being exposed to spores sent through the mail, and five of those infected died.
More recently, in two separate outbreaks, heroin users in Europe contracted anthrax by injecting illegal drugs. A total of 40 people died. Heroin sold in Europe likely comes from areas where naturally occurring anthrax is more common.
Risk factors
To become infected with anthrax, you must come into direct contact with anthrax spores. This is more likely if you:
- Sind beim Militär und werden in einem Gebiet eingesetzt, in dem ein hohes Milzbrandrisiko besteht
- Arbeiten Sie mit Anthrax in einer Laborumgebung
- Handhaben Sie Tierhäute, Felle oder Wolle aus Gebieten mit hohem Anthrax-Vorkommen
- Arbeiten Sie in der Veterinärmedizin, insbesondere wenn Sie mit Nutztieren zu tun haben
- Behandeln oder kleiden Sie Wildtiere – während Anthrax in den Vereinigten Staaten selten ist, kommt es gelegentlich zu Ausbrüchen bei Hausrindern und Wildtieren wie Hirschen
- Injizieren Sie illegale Drogen wie Heroin
Complications
The most serious complications of anthrax include:
- Ihr Körper kann nicht normal auf eine Infektion reagieren, was zu einer Schädigung mehrerer Organsysteme führt (Sepsis)
- Entzündung der Membranen und der Flüssigkeit, die das Gehirn und das Rückenmark bedecken, was zu massiven Blutungen (hämorrhagische Meningitis) und Tod führt
prevention
To prevent infection after exposure to anthrax spores, the Centers for Disease Control and Prevention recommends:
- Eine 60-tägige Behandlung mit Antibiotika – Ciprofloxacin, Doxycyclin und Levofloxacin sind für Erwachsene und Kinder zugelassen
- Eine Reihe von Anthrax-Impfstoffen mit drei Dosen
- In einigen Fällen Behandlung mit monoklonalen Antikörpern – Raxibacumab und Obiltoxaximab
Anthrax vaccine
Anthrax vaccination is available for certain groups of people. The vaccine does not contain live bacteria and cannot cause an infection. However, the vaccine can cause side effects ranging from pain at the injection site to more serious allergic reactions.
The vaccine is not intended for the general public. Instead, it is reserved for military personnel, scientists who work with anthrax and people in other high-risk jobs.
Avoidance of infected animals
If you live or travel in a country where anthrax is widespread and herd animals are not routinely vaccinated, avoid contact with livestock and animal skins as much as possible. Also avoid eating meat that has not been cooked properly.
Even in developed countries, it is important to handle any dead animal carefully and to take precautions when working with or processing imported hides, furs or wool.
Sources:
- Wilson KH. Klinische Manifestationen und Diagnose von Anthrax. https://www.uptodate.com/contents/search. Abgerufen am 6. Februar 2020.
- Anthrax: Wie Menschen infiziert werden. Zentren für die Kontrolle und Prävention von Krankheiten. https://www.cdc.gov/anthrax/basics/how-people-are-infected.html. Abgerufen am 10. Februar 2020.
- Milzbrand. Merck Manual Professional-Version. https://www.merckmanuals.com/professional/infectious-diseases/gram-positive-bacilli/anthrax. Abgerufen am 10. Februar 2020.
- Wilson KH. Mikrobiologie, Pathogenese und Epidemiologie von Anthrax. https://www.uptodate.com/contents/search. Abgerufen am 10. Februar 2020.
- Wilson KH. Vorbeugung von Anthrax. https://www.uptodate.com/contents/search. Abgerufen am 6. Februar 2020.
- Wilson KH. Behandlung von Anthrax. https://www.uptodate.com/contents/search. Abgerufen am 6. Februar 2020.
- Stone CK, et al., Hrsg. Nukleare, biologische und chemische Kampfstoffe; Massenvernichtungswaffen. In: Aktuelle Diagnose & Behandlung Notfallmedizin. 8. Aufl. McGraw-Hill-Bildung; 2017. https://accessmedicine.mhmedical.com. Abgerufen am 10. Februar 2020.
- Fragen Sie MayoExpert. Milzbrand. Mayo-Klinik; 2019.
- Anthrax-Impfung: Was Sie wissen müssen. Zentren für die Kontrolle und Prävention von Krankheiten. https://www.cdc.gov/vaccines/hcp/vis/vis-statements/anthrax.html. Abgerufen am 7. Februar 2020.
- Anthrax: Grundlegende Informationen. Zentren für die Kontrolle und Prävention von Krankheiten. https://www.cdc.gov/anthrax/basics/index.html. Abgerufen am 12. Februar 2020.
- Impfempfehlungen gegen Milzbrand. Zentren für die Kontrolle und Prävention von Krankheiten. https://www.cdc.gov/vaccines/vpd/anthrax/hcp/recommendations.html. Abgerufen am 17. Februar 2020.

 Suche
Suche
 Mein Konto
Mein Konto