Unveiling the secrets of the pancreas: 3D imaging redefines islet cell distribution
New insights into the pancreas through 3D imaging! Researchers uncover the distribution of islet cells and revolutionize diabetes research.
Unveiling the secrets of the pancreas: 3D imaging redefines islet cell distribution
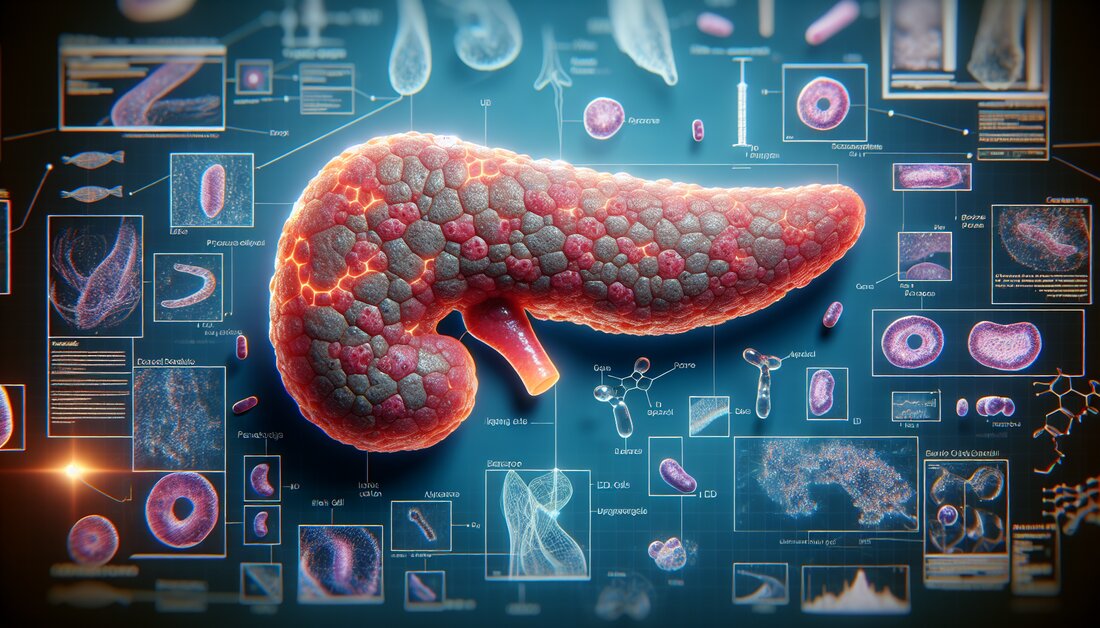
Researchers at Umeå University have managed to image an entire human organ, a pancreas, in microscopic resolution. By staining different cell types with antibodies and then examining the entire organ using 3D optical imaging techniques, their data provides a partially new picture of the pancreas. The results can be of great importance for diabetes research, especially in the development of various new treatments.
The pancreas is a key organ in the development of diabetes, a disease that affects over half a billion people today. It contains millions of small cell groups, the so-called islets of Langerhans, whose job is to regulate blood sugar levels in the body. The islets contain mainly beta and alpha cells, which produce the hormones insulin and glucagon, respectively. Insulin is released into the bloodstream and acts like a key that unlocks the body's cells so they can absorb sugar (glucose), the body's main form of energy, after a meal. Glucagon, in turn, releases glucose stores when we need energy. Glucagon, in turn, releases glucose stores when cells need energy. These two cell types also communicate directly with each other to optimize proper glucose levels in the body.
Both insulin and glucagon cells were discovered over a hundred years ago and it was long believed that the islets should contain both cell types to form a fully functional unit.
Ulf Ahlgren, Professor, Department of Medical and Translational Biology
Difficult to study
Because the islets of Langerhans make up only a few percent of the pancreas despite being so numerous, it has historically been very difficult to examine them directly in the pancreas. In most cases, researchers have had to examine tissue sections that only provide a 2D image of a very small portion of the organ. Now Umeå researchers have used 3D optical techniques that can label different cell types with fluorescently colored antibodies.
Entire organ in microscopic resolution
"By breaking the entire organ into smaller pieces, we allow the antibodies to get where they need to go. Because we know where each piece comes from, we can then, after scanning the different parts individually, 'put the entire pancreas back together.' This allows us to perform a variety of calculations and study what types of cells are present and where they are located in 3D space, as we know the 3D coordinates, their volume, shape and other parameters for every single contaminated object throughout the organ.”
New perspective on island cellularity
In addition to new data on how insulin-producing cells are distributed in the pancreas, researchers now show that glucagon-producing cells are not present in up to 50% of the islets of Langerhans, which contain insulin cells. This is in contrast to what was previously thought, where islets were thought to contain both insulin- and glucagon-expressing cell types with the same islet.
This was a surprise for us and I believe that these results could be of great importance for diabetes research. First, it shows that the islands have a much more patchy composition or cellularity than previously thought. This could mean that islands of different composition are specifically specialized to respond to different signals and/or to operate in different metabolic environments. Of course we really want to find out,” says Ulf Ahlgren.
"Second, much of the research in diabetes is conducted on isolated islets of Langerhans from deceased donors. Since we also show that this uneven composition is largely related to islet size, this means that the results of such experiments may not be fully reflective." how the islets in the living pancreas are structured and function. This could potentially be important for everything from islet transplants for type 1 diabetes to studies trying to create islets of Langerhans from stem cells.
Basis for future studies
The research team will now continue to work on whether their methods can be used to determine whether other cell types in the pancreas are also involved in the formation of the islets in a previously unknown way. In addition, they will investigate whether things are similar in mouse models, which could impact the use of mice for preclinical diabetes research.
“The methods and data that we are now publishing can form an important basis for future studies on human material to better understand what happens in the pancreas during the development of type 1 and type 2 diabetes, but also in diseases such as pancreatic cancer,” says Ulf Ahlgren.
The results are published in the journal Nature Communications. The authors of the article are Joakim Lehrstrand, Wayne Davies, Max Hahn, Tomas Alanentalo and Ulf Ahlgren, all from the Department of Medical and Translational Biology at Umeå University, and Olle Korsgren from the Department of Immunology, Genetics and Pathology at Uppsala University.
Sources:
Lehrstrand, J.,et al.(2024). Illuminating the complete ß-cell mass of the human pancreas-signifying a new view on the islets of Langerhans. Nature Communications. doi.org/10.1038/s41467-024-47686-7.

 Suche
Suche
 Mein Konto
Mein Konto